 By Lauren Christene Strazzulla
By Lauren Christene Strazzulla
Peer Reviewed
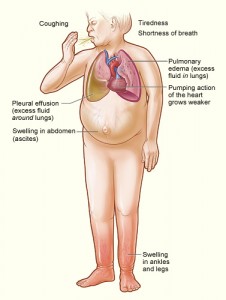
The lifetime risk for developing heart failure from age 55 on is 33% for men and 28.5% for women, and as the population ages, there is an increasing prevalence of this disease along with its associated health care costs [1, 2]. Heart failure is divisible into 2 distinct entities: those with left ventricular systolic dysfunction and those with cardiovascular compromise that does not decrease LV ejection fraction, which is termed heart failure with persevered ejection fraction (HFpEF) [3]. While these 2 subgroups may present similarly, they develop through different pathophysiological mechanisms.
In heart failure with reduced ejection fraction (HFrEF), systolic function is impaired [4]. On the other hand, HFpEF is a heterogeneous and poorly understood condition, and its exact causes remain unclear. A combination of myocardial hypertrophy, decreased vascular compliance, and prolonged vascular relaxation likely contribute to the diastolic dysfunction found in HFpEF [5]. Patients with HFrEF are typically managed with proven medical therapies, including beta-blockers, which offer significant improvement in all-cause and cardiovascular mortality and morbidity, according to randomized control trials [6]. Though there is high morbidity and mortality associated with HFpEF, the only medication definitively recommended by ACCF/AHA practice guidelines are diuretics for volume optimization [7]. Currently, the evidence in support of beta-blocker use in HFpEF patients remains controversial.
Beta-blockers were initially considered to be the drug of choice for HFrEF based on the observation that excessive beta-adrenergic stimulation of myocytes can lead to dysfunction and death at the cellular level [7-9]. The decrease in adrenergic tone caused by beta-blockers also leads to a reduction in heart rate, which has important clinical consequences. A 2009 meta-analysis examined the role of beta-blockers in patients with heart failure, 95% of whom had a reduced ejection fraction. This investigation showed that the survival benefit for beta-blockers is associated with the magnitude of the reduction in heart rate but not the drug dosage [10]. Similarly, at least 3 large randomized control studies conducted in the United States, testing bisoprolol, carvedilol, and metoprolol in over 10,000 patients with HFrEF, have confirmed the mortality benefit of using these medications for this subset of heart failure patients [11].
In contrast, beta-blockers are more controversial and may even be detrimental in HFpEF. Borlaug et al. demonstrated that during exercise, patients with HFpEF achieved an inadequate chronotropic response and consequently were not able to increase their cardiac output appropriately despite a similar rise in end diastolic volume, stroke volume, and contractility compared to those with hypertensive cardiac hypertrophy. Importantly, these patients exhibited delayed heart rate decline after exercise, which is a predictor of overall mortality [12, 13]. This data calls into question the potential harmful effects of heart rate reducing medications in patients with HFpEF, who may already have reduced chronotropic reserve and poor exercise capacity [14].
Though some studies have suggested a mortality benefit for beta-blockers in HFpEF, it is unclear how to interpret these studies. For example, the findings from an open-label randomized controlled trial of patients with HF and an LVEF ≥ 40%, demonstrated that those who received propranolol had a 35% lower risk of mortality at 32 months compared with those who did not. However, this was a small study (158 subjects), and prior myocardial infarction was a mandatory inclusion criterion in this study. Given that beta-blockers are known to improve outcomes after myocardial infarction, it is not certain if this study proves a mortality benefit for beta-blockers specific to HFpEF patients [15]. Another randomized study, SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors with Heart Failure), investigated the role of nebivolol in preventing the primary endpoint of all-cause mortality or cardiovascular hospitalizations in over 2,000 elderly patients, one third of whom had an EF > 35%. Nebivolol was found to reduce the risk of either mortality or cardiovascular hospitalizations in both subgroups with impaired EF (≤ 35%) and preserved EF (> 35%) [16]. These results imply that the known benefit of beta-blockers in HFrEF patients can be applied to HFpEF patients as well. But the implications of this study have been questioned, because nebivolol has unique vasodilatory effects not found in other beta-blockers, and the cutpoint for “preserved” EF was low (35%) [17].
While there have been no large randomized trials of beta-blockers specifically in HFpEF patients, the extensive OPTIMISE-HF registry tracked outcomes in a total of over 7,000 elderly patients who were hospitalized with a diagnosis of heart failure. This study found that beta-blockers did not significantly affect mortality or rehospitalization risks among those with preserved systolic function [18]. In 2015, Bavishi et al conducted a systematic review and meta-analysis encompassing 17 studies (15 of which were observational) and 27,099 patients with HFpEF. Their results revealed a 19% reduction in all-cause mortality among those taking beta-blockers, but subgroup analysis showed no effect in the elderly over 75 years of age. Furthermore, beta-blockers were not shown to improve HF hospitalization rates in HFpEF patients [19].
Given the unclear disease mechanisms underlying HFpEF, it is possible that different groups of these patients may have varied responses to beta-blockers. For example, in a prospective observational study, beta-blockers prescribed at hospital discharge in HFpEF patients were significantly associated with a higher risk of HF rehospitalization in female but not male patients [20]. Notably, patients with HFpEF are more likely to be elderly, be female, and have other comorbidities, including hypertension, ventricular hypertrophy, diabetes, sleep apnea, and obesity [21]. Until there is a more conclusive answer on the use of beta-blockers in these patients, most physicians recommend focusing management on treating these associated comorbidities, which are more likely to impact clinical outcomes in patients with HFpEF [4, 7].
Lauren Christene Strazzulla is a 4th year medical student at NYU Langone Health
Peer reviewed by Robert Donnino, MD, Cardiology Editor, Clinical Correlations
Image courtesy of Wikimedia Commons
References:
[1] G. S. Bleumink, A. M. Knetsch, M. C. J. M. Sturkenboom et al., “Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure,” European heart journal, vol. 25, no. 18, pp. 1614-1619, 2004. https://www.ncbi.nlm.nih.gov/pubmed/15351160
[2] T. Thom, N. Haase, W. Rosamond et al., “Heart disease and stroke statistics—2006 update a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee,” Circulation, vol. 113, no. 6, pp. e85-e151, 2006.
[3] J. S. Borer, and L. Tavazzi, “Update on ivabradine for heart failure,” Trends Cardiovasc Med, Jan 28, 2016. http://www.tcmonline.org/article/S1050-1738(16)00022-0/fulltext
[4] H. Iwano, and W. C. Little, “Heart failure: what does ejection fraction have to do with it?,” J Cardiol, vol. 62, no. 1, pp. 1-3, Jul, 2013.
[5] A. Abbate, R. Arena, N. Abouzaki et al., “Heart failure with preserved ejection fraction: refocusing on diastole,” International journal of cardiology, vol. 179, pp. 430-440, 2015.
[6] S. Chatterjee, G. Biondi-Zoccai, A. Abbate et al., “Benefits of β blockers in patients with heart failure and reduced ejection fraction: network meta-analysis,” 2013.
[7] C. W. Yancy, M. Jessup, B. Bozkurt et al., “2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines,” Journal of the American College of Cardiology, vol. 62, no. 16, pp. e147-e239, 2013. https://www.ncbi.nlm.nih.gov/pubmed/23741058
[8] J. J. V. McMurray, “Systolic heart failure,” New England Journal of Medicine, vol. 362, no. 3, pp. 228-238, 2010.
[9] J. J. V. McMurray, S. Adamopoulos, S. D. Anker et al., “ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012,” European journal of heart failure, vol. 14, no. 8, pp. 803-869, 2012.
[10] F. A. McAlister, N. Wiebe, J. A. Ezekowitz et al., “Meta-analysis: β-blocker dose, heart rate reduction, and death in patients with heart failure,” Annals of Internal Medicine, vol. 150, no. 11, pp. 784-794, 2009.
[11] J. M. Foody, M. H. Farrell, and H. M. Krumholz, “β-Blocker therapy in heart failure: scientific review,” Jama, vol. 287, no. 7, pp. 883-889, 2002. https://www.ncbi.nlm.nih.gov/pubmed/11851582
[12] B. A. Borlaug, V. Melenovsky, S. D. Russell et al., “Impaired chronotropic and vasodilator reserves limit exercise capacity in patients with heart failure and a preserved ejection fraction,” Circulation, vol. 114, no. 20, pp. 2138-2147, 2006.
[13] C. R. Cole, E. H. Blackstone, F. J. Pashkow et al., “Heart-rate recovery immediately after exercise as a predictor of mortality,” New England Journal of Medicine, vol. 341, no. 18, pp. 1351-1357, 1999.
[14] A. Deswal, and B. Bozkurt, “Treatment of patients with heart failure and preserved ejection fraction,” Curr Treat Options Cardiovasc Med, vol. 10, no. 6, pp. 516-28, Dec, 2008. https://www.ncbi.nlm.nih.gov/pubmed/19026182
[15] W. S. Aronow, C. Ahn, and I. Kronzon, “Effect of propranolol versus no propranolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction≥ 40% treated with diuretics plus angiotensin-converting enzyme inhibitors,” The American journal of cardiology, vol. 80, no. 2, pp. 207-209, 1997.
[16] D. J. van Veldhuisen, A. Cohen-Solal, M. Böhm et al., “Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction: Data From SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors With Heart Failure),” Journal of the American College of Cardiology, vol. 53, no. 23, pp. 2150-2158, 2009.
[17] M. El-Refai, E. L. Peterson, K. Wells et al., “Comparison of beta-blocker effectiveness in heart failure patients with preserved ejection fraction versus those with reduced ejection fraction,” J Card Fail, vol. 19, no. 2, pp. 73-9, Feb, 2013. https://www.ncbi.nlm.nih.gov/pubmed/23384631
[18] A. F. Hernandez, B. G. Hammill, C. M. O’Connor et al., “Clinical effectiveness of beta-blockers in heart failure: findings from the OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure) Registry,” Journal of the American College of Cardiology, vol. 53, no. 2, pp. 184-192, 2009.
[19] C. Bavishi, S. Chatterjee, S. Ather et al., “Beta-blockers in heart failure with preserved ejection fraction: a meta-analysis,” Heart Fail Rev, vol. 20, no. 2, pp. 193-201, Mar, 2015.
[20] S. M. Farasat, D. T. Bolger, V. Shetty et al., “Effect of Beta-blocker therapy on rehospitalization rates in women versus men with heart failure and preserved ejection fraction,” Am J Cardiol, vol. 105, no. 2, pp. 229-34, Jan 15, 2010.
[21] D. W. Kitzman, J. M. Gardin, J. S. Gottdiener et al., “Importance of heart failure with preserved systolic function in patients≥ 65 years of age,” The American journal of cardiology, vol. 87, no. 4, pp. 413-419, 2001. https://www.ncbi.nlm.nih.gov/pubmed/11179524
