Vivian Hayashi MD and Robert Smith MD, Mystery Quiz Section Editors
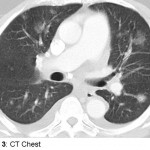
The patient is a 74 year old man complaining of hemoptysis for four days. The patient has a history of hypertension, but had not been followed medically for many years until two weeks earlier when he presented with leg swelling, breathlessness, and atrial flutter. He was admitted, diuresed, begun on antihypertensive medications including hydralazine, aspirin, and anti-coagulated with enoxaparin and warfarin. After discharge, the patient felt well for a few days before the onset of hemoptysis. There was no associated fever, chest pain, arthralgias, headaches, or visual changes. On this admission, the patient did not appear acutely ill. Resting pulse oximetry and vital signs were normal, except for a mildly elevated blood pressure. The chest was clear to auscultation; the lower extremities had mild pitting edema. Labs showed hemoglobin that was decreased nearly 3gm/dL from baseline; INR was 1.5; white blood cell count and serum creatinine were normal; the urinalysis was bland.