Faculty Peer Reviewed
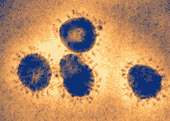
This week, captivating the interest of health and lay media alike is news of the emerging viral infection dubbed MERS-CoV (Middle Eastern Respiratory Syndrome Coronavirus). Although popular media is rife with dramatic statements such as that of Dr. Margaret Chan, Director-General of the World Health Organization, when at the 66th session of the World Health Assembly, she called it “a threat to the entire world”, we are obliged to look at the facts for ourselves. What is known currently is that the virus, first discovered in September of 2012 in Saudi Arabia, is a previously unknown member of the coronavirus family and a close phylogenetic cousin of the virus causing SARS. As of May 30, there have been 51 confirmed cases with 30 deaths. It remains to be seen whether this infection will become a pandemic, or be relegated to a footnote in history. With that in mind, let’s turn to what’s new in the literature in this week’s PrimeCuts.
A recurring question in cardiovascular research is which patients with coronary disease, including multi-vessel disease, require bypass surgery as opposed to a percutaneous intervention. In the Annals this week, a large observational study looked at 105,156 propensity-score matched patients who had received either multi-vessel CABG or multi-vessel PCI to determine differences in mortality over five years of followup [1]. In addition to a significant overall mortality benefit seen with CABG (HR 0.92), the investigators also noted a more marked benefit among certain subgroups; namely patients with diabetes, congestive heart failure, a history of tobacco use, and peripheral arterial disease. As with any cohort study, the large population studied allows the authors to answer questions that may not be amenable to a randomized control trial. This however is done at the expense of introducing unadjusted confounders that can help produce spurious results. The findings support prior meta-analyses of randomized controlled trials showing a slight benefit to CABG over PCI in an otherwise unselected patient with multi-vessel coronary disease. In addition, it confirms certain prior studies showing subgroup benefits (specifically, the FREEDOM trial in diabetics and the CASS registry in left ventricular dysfunction) [2,3]. This study does raise the question, however, of whether tobacco use or peripheral arterial disease confers an independent benefit to those undergoing CABG as opposed to PCI. Until randomized trials specifically addressing CABG vs PCI in these patients are undertaken, it may be wise to favor CABG in patients with active tobacco use or known peripheral arterial disease.
Recently, the topic of prostate cancer screening has sparked much debate, as well as changes in guidelines and clinical practice. In JAMA this week, a longitudinal cohort study followed nearly 300,000 men 65 years of age and older in the VA healthcare system to analyze not only their mortality, but the diagnostic tests to which they were subjected [4]. They found that of the men tested, 8.5% had a PSA level greater than 4. Approximately one third of those men had at least one prostate biopsy and approximately two thirds of those biopsies revealed prostate cancer. Of the men who were diagnosed with cancer, 82% underwent some form of treatment. When a diagnostic test is being evaluated for efficacy in clinical practice, it is always important for both the provider and the patient to consider the downstream testing and treatment implications. As we all know, the USPSTF officially recommended against PSA based prostate cancer screening in May 2012, and as mentioned in last week’s PrimeCuts, the AUA has begun to move away from PSA screening as well. This article highlights the underpinnings of these decisions, in that two thirds of men with an elevated PSA did not undergo any further invasive testing or treatment and had a much higher likelihood of dying from medical comorbidities unrelated to prostate disease.
Also in the realm of oncology, a report in the New England Journal this week compares crizotinib, a tyrosine kinase inhibitor, to standard chemotherapy (either pemetrexed or docetaxel) in the treatment of locally advanced or metastatic ALK-positive lung cancer (about 3-5% of all non-small-cell lung cancers) [5]. The primary outcome, median progression free survival was 7.7 months in the crizotinib group as compared to 3 months in the standard therapy group. Quality of life in the crizotinib group was also significantly higher. In the era of gene-specific chemotherapy, this represents a significant advance in the treatment of this form of cancer, hopefully on par with the use of erlotinib in EGFR-positive non-small cell lung cancers [6]. Typically, crizotinib is used as a second line chemotherapy, but with this demonstration of efficacy, may be approaching first-line status. However, the other issue common to new targeted therapies is that of cost effectiveness. Even erlotinib only extends life by 3.3 months. At a cost of nearly $10,000 for one month of treatment with crizotinib, it may be prohibitively expensive for most.
Finally, an article in the British Medical Journal this week looked at the incidence of pneumonia and its complications in 5,468 patients with COPD treated with either budesonide/formoterol or fluticasone/salmeterol [7]. In this retrospective propensity score matched study, patients treated with fluticasone/salmeterol were 1.7 times more likely to have pneumonia and be admitted to the hospital, as well as 1.7 times more likely to die from pneumonia than their budesonide/formoterol counterparts (with statistical significance achieved for those figures). These findings support previous results showing increased incidence of pneumonia in patients treated with salmeterol/fluticasone that have not been borne out in other studies involving budesonide. Given that the two drug combinations use identical drug classes, it seems more likely that this finding is due to an idiosyncrasy of fluticasone, rather than a class effect. Perhaps these findings should prompt patients with a history of pneumonia who require an inhaled corticosteroid/long acting beta agonist combination to be preferentially prescribed budesonide/formoterol.
Other interesting reads this week…
1. Peterson DC, et al. Outcomes of medical emergencies on commercial airline flights. N Engl J Med. 2013 May 30;368(22):2075-83. http://www.nejm.org/doi/full/10.1056/NEJMoa1212052
Does the thought of an airline flight fill you with a primal terror of being the only physician onboard while a passenger clutches his chest 30,000 feet over the mid-Atlantic? Worry no more! This review from the New England Journal characterizes the most common in-flight medical symptoms as syncope/pre-syncope and respiratory in nature, with only 7.3% resulting in flight diversion, and a mortality rate of only 0.3%.
2. Saint S, et al. Preventing catheter-associated urinary tract infection in the united states: a national comparative study. JAMA Intern Med. 2013 May 27;173(10):874-9. http://archinte.jamanetwork.com/article.aspx? articleid=1672273
Do you hate it when surgery consult asks you to put in a Foley catheter for accurate ins and outs? Does it just make you visualize the ESBL Klebs UTI that the patient is bound to contract? This article reviews the practices of Michigan hospitals, where a campaign to prevent catheter-associated UTIs has resulted in a 25% reduction in their incidence as compared to a 6% reduction with the rest of the United States.
3. Moran A, et al. Interleukin-1 antagonism in type 1 diabetes of recent onset: two multicentre, randomised, double-blind, placebo-controlled trials. Lancet. 2013 Apr 4. Advance online publication. doi: 10.1016/S0140-6736(13)60023-9. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(13)60023-9/fulltext
With the goal to halt the auto-immune process of type 1 diabetes before complete pancreatic beta cell destruction, two trials (one involving the anti-IL1 antibody canakinumab and the other involving the IL1 receptor antagonist anakinra) were performed in type 1 diabetics of recent onset. Unfortunately, insulin production, as measured by plasma c-peptide showed no significant difference from placebo in either group.
Dr. Matthew Vorsanger is a third-year resident at NYU Langone Medical Center
Peer reviewed by Neil Shapiro, MD, Editor-In-Chief, Clinical Correlations
Image courstesy of Wikimedia Commons
References:
1. Hlatky MA, et al. Comparative effectiveness of multivessel coronary bypass surgery and multivessel percutaneous coronary intervention: a cohort study. Ann Intern Med. 2013 May 21;158(10):727-34. http://annals.org/article.aspx?articleid=1679804
2. Faroukh ME, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367(25):2375. http://www.nejm.org.ezproxy.med.nyu.edu/doi/full/10.1056/NEJMoa1211585
3. Passamani E, et al. A randomized trial of coronary artery bypass surgery. Survival of patients with a low ejection fraction. N Engl J Med. 1985;312(26):1665. http://www.nejm.org.ezproxy.med.nyu.edu/doi/full/10.1056/NEJM198506273122603
4. Walter LC, et al. Five-year downstream outcomes following prostate-specific antigen screening in older men. JAMA Intern Med. 2013 May 27;173(10):866-73. http://archinte.jamanetwork.com/article.aspx?articleid=1678809
5. Shaw AT, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. Advance online publication. doi: 10.1056/NEJMoa1214886. http://www.nejm.org/doi/full/10.1056/NEJMoa1214886
6. Zhou C, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12(8):735. http://www.thelancet.com.ezproxy.med.nyu.edu/journals/lanonc/article/PIIS1470-2045%2811%2970184-X/fulltext
7. Janson C, et al. Pneumonia and pneumonia related mortality in patients with COPD treated with fixed combinations of inhaled corticosteroid and long acting beta-2 agonist: observational matched cohort study (PATHOS). BMJ. 2013 May 29;346:f3306. http://www.bmj.com/content/346/bmj.f3306?view=long&pmid=23719639

One comment on “Primecuts – This Week In The Journals”
Thank you so much for this very comprehensive, yet succinct approach to presenting vital, medical research and conclusions. Great article! I hope and pray the MERS-CoV will just “die out” and fade into history!
Comments are closed.