Peer Reviewed
Last Friday, Aetna and Gilead Sciences, the well-known maker of Sovaldi, the “$1000-a-pill” treatment for Hepatitis C, reached a discount agreement that will allow Sovaldi to populate Aetna’s reimbursement lists [1]. Aetna’s decision came after a thorough clinical review of all advanced treatment courses currently available on the market, most of which are priced just under the $100k mark.
Sovaldi also gained mention last week in Malcolm Gladwell’s review of “America’s Bitter Pill,” Steven Brill’s newly published account of the rocky implementation of the Affordable Care Act [2]. In the review, Gladwell frequently chides Brill for ineffective use of examples, and includes a defense against Brill’s critique of Sovaldi:
“The problem with the pharmaceutical industry is not that it makes too many drugs like Sovaldi. It’s that it makes too many drugs that aren’t like Sovaldi, drugs whose costs vastly outstrip their benefits: cancer treatments that cost tens of thousands of dollars and extend life only minimally, or expensive me-too drugs that perform no better than cheap generics.”
Gladwell brings up an important point that warrants further debate and has done so before, memorably in a controversial 2004 article defending the drug pricing schemes of the pharmaceutical industry [3]. It is worth mentioning, however, his long list of potential conflicts of interest, most notably in the form of a formidable roster of highly profitable corporate speaking engagements. After controversy emerged regarding Gladwell’s compensation for these engagements in the wake of the 2004 article, he was inspired to post a lengthy disclosure statement on his website [4].
The ongoing debate on regulation versus free market capitalism within the complex ethical web of modern healthcare is alive and well.
Elsewhere in the medical world…
Mortality and Treatment Patterns Among Patients Hospitalized With Acute Cardiovascular Conditions During Dates of National Cardiology Meetings [5].
Over the holidays, a study published online by JAMA Internal Medicine made us question how aggressively cardiac interventions should be pursued. The retrospective study looked at the 30-day mortality of patients hospitalized with a myocardial infarction (MI), heart failure, or cardiac arrest during 2 major national cardiology conferences between 2002-2011. Mortality rates were lower during times of conference attendance for heart failure (17.5% vs 24.8% ) and cardiac arrest patients (59.1% vs 69.4%), and while similar for MI patients in both groups (39.2% vs 38.5%), the conference-time group underwent less percutaneous coronary interventions (20% vs 28%).
These results suggest that modern cardiologists may be escalating to interventions with greater frequency but without commensurate mortality benefit. More conservative management may even confer a mortality benefit by eliminating complications associated with high-risk interventions. NPR and several other news venues represented the study in various shades of healthcare critique (Is Your Heart Doctor In? If Not, You Might Not Be Any Worse Off [6]). In an editor’s note, Dr. Rita Redberg comments: “It is reassuring that patient outcomes do not suffer while many cardiologists are away. More important, this analysis may help us to understand how we could lower mortality throughout the year” [7].
Community-Wide Cardiovascular Disease Prevention Programs and Health Outcomes in a Rural County, 1970-2010 [8]
Shifting the focus over from intervention to prevention, an article published in JAMA this week describes the effectiveness of a 40-year-long sustained group of community prevention programs targeted to reduce the risk of cardiovascular disease in Franklin County, Maine. The programs produced significant improvements for the examined time intervals in hypertension control (18.3% to 43.0%), cholesterol control (0.4% to 28.9%), smoking quit rates (48.5% to 69.5%), hospitalizations per capita (17 less per 1k residents), and overall mortality (60 less deaths per 100k residents). The authors suggest that further research and development is needed to establish generalizable principles of program design that cater to a more diverse selection of community groups in the US and eventually the rest of the world. These results are a robust reminder that prevention remains far-and-away our most effective (and often insufficiently explored) tool in cardiovascular disease risk reduction.
Crohn’s disease management after intestinal resection: a randomised trial [9]
Patients with Crohn’s disease are plagued with significant lifetime morbidity: many require intestinal resection, and there are still high rates of recurrence following surgery. A study coming out in The Lancet aims to establish the benefit of early surveillance colonoscopy and aggressive treatment step-up for recurrence in Crohn’s patients after initial intestinal resection. The subjects were randomized at 6 months post-operatively to either receive surveillance colonoscopy or standard non-invasive clinical surveillance. If deemed to have recurrence, patients received additional immune suppressive therapy with thiopurine and/or adalimumab. Outcomes were measured at 18 months, with the early colonoscopy group seeing benefits in lower recurrences (49% vs 67%) as well as in complete mucosal normality (22% vs 8%). Early surveillance with standardized colonoscopy in addition to clinical judgement, aggressive escalation of medical treatment based on results, and periodic future monitoring all appear to be keys to reducing morbidity from recurrence in Crohn’s.
Trends in Opioid Analgesic Abuse and Mortality in the United States [10]
Frequently, physicians summon an inner calm during their busy days and take time to combat the persistent, often subversive, complicated psychology of the drug-seeking patient. In NEJM this week, a study looks at trends in abuse of the six most commonly prescribed opioids in the Unites States (oxycodone, hydrocodone, hydromorphone, fentanyl, morphine, and tramadol) from 2002-2013 using data from the Researched Abuse, Diversion, and Addiction-Related Surveillance (RADARS) System. The period 2002-2010 was a problematic time during which the United States experienced a profound increase in opioid prescriptions, diversion and abuse of the medications, and commensurately an increase in mortality attributable to opioid abuse. Between 2011-2013, however, the aforementioned measures have all plateaued and many have even started to decrease. It is possible that the relatively recent arsenal of federal and state tools designed to detect and prevent opioid abuse (such as the ISTOP registry familiarly implemented across NYU hospitals) is finally taking effect. Let’s keep up the good work.
Other tidbits…
Hospital Variation in Quality of Discharge Summaries for Patients Hospitalized With Heart Failure Exacerbation [11]
Discharge summaries are frequently rushed or procrastinated, and are notorious for piling up at the end of a resident physician’s day. This study published by NYU faculty member Dr. Leora Horowitz et al examines why more emphasis needs to go toward promoting safe and effective discharge summary composition, and how to initiate the change.
End-of-Life Care in the Intensive Care Unit: How Asia Differs From the West [12]
In the ongoing discussion regarding the role of Palliative Care in the ICU, this study examines opinions in Asia vs the West for differences in the threshold for withdrawal of care, patient and family expectations, and physicians’ perception of the ethical weight of different forms of care withdrawal (such as initially withholding vs implementing then withdrawing).
Multiple Myeloma [13]
Remember what the mnemonic C.R.A.B. stands for? Always having to go back and google the interpretation of SPEP/UPEP test results? This excellent JAMA review article on multiple myeloma is just the reference for brushing up on the pathophysiology and diagnosis of MM, as well as staying up to date with several promising new treatments.
Dr. Jovan Begovic is a 1st year resident at NYU Langone Medical Center
Peer reviewed by Anish B. Parikh, MD, 3rd year resident at NYU Langone Medical Center
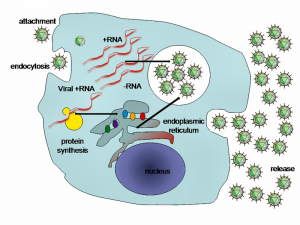
Image courtesy of Wikimedia Commons
References:
[1] http://www.reuters.com/article/2015/01/16/us-healthcare-aetna-hepatitisc-idUSKBN0KP28O20150116
[2] http://www.newyorker.com/magazine/2015/01/12/bill-6
[3] http://www.newyorker.com/magazine/2004/10/25/high-prices
[4] http://gladwell.com/disclosure-statement/
[5] http://archinte.jamanetwork.com/article.aspx?articleid=2038979
[7] http://archinte.jamanetwork.com/article.aspx?articleid=2038976
[8] http://jama.jamanetwork.com/article.aspx?articleid=2089352
[9] http://www.sciencedirect.com/science/article/pii/S0140673614619085
[10] http://www.nejm.org/doi/full/10.1056/NEJMsa1406143?query=featured_home
[11] http://circoutcomes.ahajournals.org/content/early/2015/01/13/CIRCOUTCOMES.114.001227.abstract
[12] http://archinte.jamanetwork.com/article.aspx?articleid=2089228
[13] http://www.sciencedirect.com/science/article/pii/S0140673614604931