Peer Reviewed
You can get a Botox injection almost anywhere these days. Internists, dermatologists, and even gynecologists have capitalized on an aging group of baby boomers who aren’t fans of their wrinkles. And it’s true that with an impressive safety profile, few contraindications, rapid effectiveness, and positive cash return for providers, botulinum toxin injections for cosmetic purposes can make everyone happy.
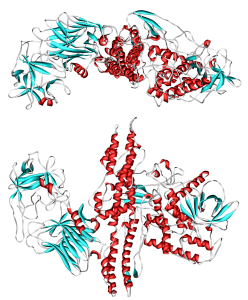
Botulinim toxin is produced by the anaerobic bacterium, Clostridium botulinum. This is the strongest toxin found in nature. When injected into muscle, it is taken up by neurons via endocytosis, and then travels to the neuromuscular junction and prevents calcium-dependent release of acetylcholine [1]. This blocks nerve impulses, resulting in flaccid paralysis of the injected muscle.
Facial wrinkles are caused by dermal atrophy and repetitive contraction of the underlying facial muscles, especially around the forehead and periocular areas [2]. Injection of botulinum toxin into specific overactive muscles causes relaxation, and subsequent smoothing over the overlying skin. This procedure is FDA-approved, has predictable results and few adverse events, and is generally associated with high patient satisfaction [2]. For these reasons, botulinum toxin injections for frown lines and crow’s feet are among the most common dermatologic procedures performed in this country.
Yet, the powerful neuromuscular blocking agent has many non-cosmetic uses. Many specialties of medicine, including neurology and urology, have capitalized on botulinum toxin’s ability to selectively paralyze small muscles. In particular, it is frequently used for the treatment of another common problem: migraine.
Botulinum toxin has the ability to block the release of many pain neurotransmitters, including substance P, glutamate, and calcitonin gene-related peptide (CGRP) from the pre-synaptic nerve terminal [3]. The details surrounding this are poorly understood, but some evidence suggests that the toxin can diffuse into the nerve endings and inhibit neurotransmitter release to modulate pain at the level of the trigeminal-occipital-cervical complex [4]. The analgesic effects of botulinum toxin injections are well established, both within clinical trial data and anecdotally; these effects are distinctly different from those of muscle relaxation [4]. Although data on the use of botulinum toxin in episodic migraine were inconclusive, more promising results have been shown for its use in individuals suffering from chronic migraine. In the PREEMPT 1 and 2 studies, onabotulinum toxin A was shown to be significantly superior to placebo with regard to decreasing the frequency of headache days in patients with chronic migraine [4, 5]. It was also shown to be safe and well-tolerated. The FDA approved botulinum toxin as a treatment for chronic migraine in May 2013 [6].
Practically, treatment of migraine with botulinum toxin targets the supraorbital, supratrochlear, and auriculotemporal branches of the trigeminal nerve [4]. These peripheral sensory nerves are accessed by injecting the procerus, corrugator, and frontalis muscles in the forehead – many of the same muscles that are injected for cosmetic purposes. It is also common practice to inject the neck and shoulder region to target cervical sensory rami from C2, C3, C4, and C5 [4].
Botulinum toxin is also used in the treatment of cervical dystonia. Also known as spasmodic torticollis, this is a focal dystonia characterized by abnormal cervical muscle spasms causing significant pain and involuntary posturing of the head and neck. The most common muscles involved are the sternocleidomastoid, trapezius, and splenius capitus, although the scalenes and platysma may also be involved [7]. By blocking the release of acetylcholine at the neuromuscular junction, the toxin has the ability to temporarily weaken the muscle in spasm, alleviate the associated pain, and correct posture. In a double-blind, placebo-controlled trial, onabotulinum toxin A produced significant improvement in the severity of torticollis and in the disability and pain associated with it [8]. While generally safe for this indication, dysphagia is commonly reported, especially for individuals whose dystonia requires injection of the sternocleidomastoid and/or platysma muscles. Also, patients with pre-existing swallowing or breathing disorders are more susceptible to dysphagia [14]. Dry mouth and muscle weakness have also been reported, although these side effects vary based on formulation and dose [7]. Whereas many cases of cervical dystonia are refractory to systemic medications like anticholinergics, baclofen, skeletal muscle relaxants, and benzodiazepines—all of which come with potentially serious side effects—botulinum toxin is now considered first-line treatment. It is also FDA-approved for blepharospasm and other focal spasticities, including upper and lower extremity muscle spasticity following stroke, or in children with cerebral palsy.
A less intuitive use for botulinum toxin is the treatment of hyperhidrosis. More commonly known as excessive sweating, hyperhidrosis is an autonomic and typically idiopathic disorder that can lead to social embarrassment and occupational and psychological disability [9]. Although it most commonly occurs in the axillary region, it can also be seen in the palms, soles, and groin. As discussed above, onabotulinum toxin A inhibits release of acetylcholine from the sympathetic nerve endings, thereby effectively paralyzing eccrine glands. Accordingly, local injection of the toxin directly into the axilla has been shown to significantly reduce sweating in multiple clinical trials [10]. Botulinum toxin is FDA-approved as first-line therapy for patients with severe axillary hyperhidrosis and as second-line therapy in those who have failed alternative treatments [11].
Botulinum toxin also has several indications in the genitourinary realm. In particular, it is effective in treating detrusor muscle overactivity, the most common culprit of urge incontinence. Although occasionally due to neurologic disease, involuntary contractions of the detrusor muscle are commonly idiopathic [12]. While first-line treatment for overactive bladder is lifestyle changes and behavioral therapy, botulinum toxin can also be used in those patients whose symptoms are refractory to more conservative measures. A major limitation, however, is urinary retention, not surprisingly caused by detrusor muscle paralysis secondary to toxin injection [12]. In a randomized, double blind, placebo-controlled trial of botulinum toxin A for refractory overactive bladder, 27% of participants experienced post-void residuals of greater than 200 cc of urine at 6 weeks of follow up, including some who required intermittent self-catheterization [13]. Urinary infection and hematuria have also been reported, but in general, patient satisfaction remains high. Botulinum toxin has also been used for benign prostatic hypertrophy, excessive urethral sphincter tone, and pelvic floor dysfunction [12]. More studies are needed to determine the toxin’s precise role in other genitourinary conditions, such as vaginismus.
The effects of botulinum toxin injection typically last 3-4 months, regardless of the anatomical site [14]. Although there are few safety risks, it may rarely cause anaphylaxis or other allergic reactions. If used in very high doses or very frequently, antibodies may form which can reduce the effectiveness of future injections, though this depends on the specific toxin utilized [14]. As with any injection, there may be lingering pain and redness at the injection site. Contraindications include hypersensitivity to botulinum toxin, active infection at the injection site, and concurrent urinary retention or infection in patients receiving a detrusor injection [14]. Furthermore, there could be specific adverse reactions based on the targeted muscle group: dysphagia after injections in the platysma or sternocleidomastoid and urinary retention for injections in the detrusor muscle [14], as discussed above. There is a phenomenon known as “spread of toxin effect” where its effects are observed beyond the site of local injection; this is rare and poorly understood, but seen most commonly in children treated for spasticity [14].
This review has only skimmed the surface of the potential uses for botulinum toxin in modern medicine. It has been studied as an alternative to surgery in patients with achalasia [15]. It has been used to manage painful muscle contraction in neurological conditions like cerebral palsy and tardive dyskinesia. It has been shown to be effective in the management of strabismus [17]. It has been used off-label to manage a wide range of conditions from trigeminal neuralgia to temporomandibular joint syndrome to anal fissures. While botulinum toxin remains most recognized for its cosmetic uses, its effects extend far beyond frown lines, and much work is needed to fully elucidate its potential for alternative therapeutic medical uses.
Dr. Samantha Kass Newman is an internal medicine resident at NYU Langone Medical Center
Peer reviewed by Jason Siefferman, MD, Anesthesiology, NYU Langone Medical Center
Image courtesy of Wikimedia Commons
References
- Montecucco C, Molgó J. Botulinal neurotoxins: revival of an old killer. Current Opinion in Pharmacology. 2005; (3): 274–279. https://www.researchgate.net/publication/7833487_Botulinal_neurotoxins_revival_of_an_old_killer_Curr_Opin_Pharmacol_5274-279
- Small R. Botulinim toxin injection for facial wrinkles. Am Fam Physician. 2014 Aug 1:90(3):168-75. http://www.aafp.org/afp/2014/0801/p168.html
- Ashkenazi A, Blumenfeld A. OnabotulinumtoxinA for the treatment of headache. Headache. 2013 Sep; 54 Suppl 2:54-61. http://www.ncbi.nlm.nih.gov/pubmed/24024603
- Szok D, Csati A, Vecsei L, Tajti J. Treatment of chronic migraine with onabotulinumtoxinA: mode of action, efficacy, and safety. Toxins (basel). 2015 Jul 17; 7(7):2659-73.
- Aurora SK, Dodick DW, Turkel CC, et al. OnabotulinumtoxinA for treatment of chronic migraine: Results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 1 trial. Cephalalgia. 2010;30:793-803. http://www.ncbi.nlm.nih.gov/pubmed/20487038
- FDA approves Botox to treat chronic migraine. Available at: http://www.fda.gov/NewsEvents/ Newsroom/PressAnnouncements/ucm229782.htm 2013. (accessed May 11, 2013)
- Mills RR and Pagan FL. Patient considerations in the treatment of cervical dystonia: focus on botulinum toxin type A. Patient Prefer Adherence. 2015; 9: 725–731.
- Greene P, Kang U, Fahn S, Brin M, Moskowitz C, Flaster E. Double-blind, placebo-controlled trial of botulinum toxin injections for the treatment of spasmodic torticollis. Neurology. 1990 Aug; 40(8):1213-8.
- Lakrai AA, Moghimi N, Jabbari B. Hyperhidrosis: anatomy, pathophysiology and treatment with emphasis on the role of botulinum toxins. Toxins (Basel). 2013 Apr 23:5(4):821-40.
- de Almeida AR, Montagner S. Botulinum toxin for axillary hyperhidrosis. Dermatol Clin. 2014 Oct. 32(4):495-504.
- An JS, Hyun Won C, Si Han J, Park HS, Seo KK. Comparison of OnabotulinumtoxinA and RimabotulinumtoxinB for the Treatment of Axillary Hyperhidrosis. Dermatol Surg.2015 Aug;41(8):960-7. http://www.nejm.org/doi/full/10.1056/NEJM200102153440704
- Apostolidis A, Dasgupta P, Denys P, et al. Recommendations on the use of botulinum toxin in the treatment of lower urinary tract disorders and pelvic floor dysfunctions: a European consensus report. Eur Urol. 2009; 55:100.
- Flynn MK, Amundsen CL, Perevich M, Liu F, Webster GD. Outcome of a randomized, double-blind, placebo controlled trial of botulinum A toxin for refractory overactive bladder. J Urol. 2009;181(6):2608.
- Botox (OnabotulinumtoxinA) [prescribing information]. Irvine, CA: Allergan; April 2015. http://www.allergan.com/assets/pdf/botox_pi.pdf
- Zhu Q, Liu J, Yang C. Clinical study on combined therapy of botulinum toxin injection and small balloon dilation in patients with esophageal achalasia. Dig Surg. 2009;26(6):493.
- Jost WH, Benecke R, Hauschke D, Jankovic J, Kaňovský P, Roggenkämper P, Simpson DM, Comella CL. Clinical and pharmacological properties of incobotulinumtoxinA and its use in neurological disorders. Drug Des Devel Ther. 2015 Apr 1;9:1913-26
- Donahue SP. Botulinum toxin treatment for esotropia. Am Orthopt J. 2013(63):29-31. http://www.nzosi.com/uploads/1/0/2/6/10263349/botox_4_and_against_in_eso_aoj_2014.full1.pdf