Peer Reviewed
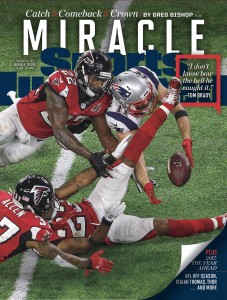
Let’s talk about that game: whether you are a diehard sports fanatic or no know nothing about football, what happened on the evening of February 4th was truly remarkable. This was the greatest comeback (or collapse, depending how you experienced it) in all of the Big Game’s history. That night, 24, yes, 24 different championship records were broken in the two teams’ combined effort. [1] In a time when national and worldwide trends have people feeling polarized, and even disheartened, more than 111 million of us came together to witness a simple game. We celebrated, we grieved, we sat in awe as we witnessed fellow human beings perform amazing feats. And through the collective emotion of onlookers fueling the drama, we all became part of what makes sports great.
Speaking of impressive feats…this week on “Primecuts:” a powerful weapon against recurrent prostate cancer, a new disease-modifying breakthrough in sickle cell pain crises, large-scale lung cancer screening in action, and combating physician burnout.
1) Crizanlizumab for the Prevention of Pain Crises in Sickle Cell Disease [2]
Crizanlizumab is a monoclonal antibody against P-selectin, whose upregulation in endothelial cells and platelets contributes to the pathogenesis of vaso-occulsion and sickle cell-related pain crises. This study reports the results of a phase 2, multicenter, randomized, placebo-controlled, double-blind, 12-month study assessing effects of 52-weeks of crizanlizumab treatment with or without hydroxyurea on annual rates sickle cell-related pain crises.
Patients with common sickle cell genotypes, ages 16-65, who had 2 to 10 sickle cell-related pain crises in the year prior, were eligible. Patients undergoing long-term red-cell transfusion therapy were excluded. 129 patients were randomly assigned to low-dose crizanlizumab (2.5 mg/kg), high-dose crizanlizumab (5.0 mg/kg), or placebo groups. Randomization was performed with patients stratified by number of crises in the preceding year and concomitant hydroxyurea use. Patients received either two loading doses of crizanlizumab or placebo two weeks apart followed by maintenance doses every four weeks through week 50 (14 total doses).
The median crisis rate per year was 1.63 in the high-dose crizanlizumab group vs. 2.98 for placebo (45.3% lower rate with high-dose crizanlizumab, P=0.01). Median crisis rate per year among patients taking concomitant hydroxyurea was 2.43 with high-dose crizanlizumab vs. 3.58 in placebo. The median rate for patients with HbSS genotype was 1.97 (high-dose) vs. 3.01 in placebo. For patients with sickle cell disease but non-HbSS gentoypes, median crisis rate was 0.99 vs. 2.00 in placebo. Median time to first crisis was significantly longer among patient in the high-dose crizanlizumab group compared to placebo (4.07 vs. 1.38 months, P=0.001) as well as the median time to second crisis (10.32 vs. 5.09 months, P=0.02). The incidence of adverse events were similar among patients treated with crizanlizumab compared to placebo. Overall, the P-selectin inhibitor crizanlizumab was associated with lower rates of crises than with placebo, regardless of concomitant hydroxyurea use or sickle cell disease genotype.
2) Radiation with or without Anti-androgen Therapy in Recurrent Prostate Cancer[3]
Radiation therapy combined with either androgen-deprivation therapy or antiandrogen therapy prolongs survival among men with intact prostate with locally advanced diseae. [4] Whether this combination of treatment can improve overall survival in men who recur following radical prostatectomy is unknown. In this double-blind, placebo-controlled trial, 760 eligible patients with stage T2 (disease confined to prostate with positive margins) or T3 (disease extending beyond prostatic capsule) disease with no nodal involvement who had undergone radical prostatectomy with persistent/recurrent detectable PSA levels of 0.2 to 4.0 ng/mL were assigned to either salvage radiation therapy (RT) plus antiandrogen therapy (bicalutamide 150mg daily for 24 months) or RT plus placebo. The primary outcome measure was overall survival. Median follow up for the study was 13 years.
Overall survival at 12 years was 76.3% in the bicalutamide group vs. 71.3% in the placebo group (hazard ratio for death, 0.77; 95% confidence interval, 0.59 to 0.99; P=0.04). The 12-year incidence of prostate cancer death was 5.8% in the bicalutamide group vs. 13.4% for placebo (P<0.001). Cumulative metastatic prostate cancer incidence was 14.5% in the bicalutamide group vs. 23% for placebo (P=0.005). Adverse effects were similar between the groups with exception of gynecomastia (70% [bicalutamide] vs. 11% [placebo]). Overall, for patients who have biochemical recurrence of prostate cancer following radical prostatectomy, adding antiandrogen therapy to salvage radiation leads to improved overall, disease-specific, and metastasis-free survival compared to salvage radiation alone.
3) Implementation of Lung Cancer Screening in the Veterans Health Administration. [5]
After the National Lung Screening Trial (NLST) found a reduction in mortality from lung cancer of 3 deaths per 1000 high-risk individuals screened, [6] US Preventive Services Task Force recommended implementing lung cancer screening (LCS) with low-dose computed tomography (LDCT) for patients age 55-80 who are former (within the past 15 years) or current smokers with at least a 30 pack-year history. [7] Published clinical experience with the recent recommendations and guidelines have been implemented are limited. [8] This study follows the results from a 3-year Veterans Health Administration’s Lung Cancer Screening Demonstration Project (LCSDP) in 8 VA hospitals. The main goals of study were to highlight the resources necessary to implement a comprehensive LCS program, patient interest in screening, lung cancer detections and incidental findings rates.
An electronic medical record screening tool was used at eight VHAs to identify patients 55 to 80 years without a diagnosis of esophageal, liver, or pancreatic cancer or lung cancer and expected to live more than 6 months. These patients were then reviewed for smoking histories and for any further medical conditions that would preclude LCS. 2106 patients underwent LCS (2028 men and 78 women; mean [SD] age, 64.9 [5.1] years) underwent LCS. Of these patients, 1257 (59.7%) had nodules; 1184 of these patients (56.2%) required tracking with follow up scans. A total of 73 patients (3.5% of all patients screened) had findings suspicious for possible lung cancer and underwent further diagnostic evaluation. Lung cancer was confirmed for 31 (1.5%) of those patients within the 330-day follow-up period; 20 (<1%) of the cancers were stage I. The rate of false-positive test results for lung cancer was 97.5% (1226 of 1257).
Extrapolating from the patients eligible from the 8 VHA sites, close to 900, 000 VHA patients country-wide may be candidates for LCS, a wide-scale roll out of LCS will increase workload for pulmonary services following up nodules and primary care for deciding which incidental findings need further evaluation. This requires further coordination/communication among clinical services, patients, and staff. Lung cancer screening coordinators will need to be hired, as they were for this study. Additional training for primary care staff and radiologists, quality assurance measures, and possibly additional CT scanners and radiology staff to accommodate those eligible and wanting to be screened. Overall, the large-scale implementation of LCS with LDCT scans is a complex undertaking and was shown to stress the capacity of radiology, pulmonary, and primary care services for a small population of patients whose early stage lung cancers.
4) Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-analysis [9]
In the US, nearly half of practicing physicians experience burnout during their careers from excessive workload, imbalance between job demands and skills, a lack of job control, and/or prolonged work stress. [10] Interventions for burnout can be classified into physician-directed interventions (e.g. individual mindfulness or cognitive behavioral techniques) and organization-directed interventions (e.g. changes in schedule/reductions in the intensity of workload, or changes in operation practices, etc.). [11] A meta-analysis was conducted to evaluate the effectiveness of burnout interventions and whether certain interventions (physician-directed vs. organizational) were associated with improved burnout scores focused on emotional exhaustion. Burnout was measured using the Maslach Burnout Inventory (MBI) measure[12] which examines emotional exhaustion, depersonalization, and personal accomplishment.
This meta-analysis included 20 controlled interventions on 1550 physicians (mean [SD] age, 40.3 [9.5] years; 49% male). Seven studies recruited physicians working in primary care, 10 studies recruited physicians in secondary care (e.g., intensivists, oncologists, and surgeons), and 2 studies recruited a mixed sample. Physician-directed inventions showed only a very small reduction in burnout (SMD=−0.18; 95% CI, −0.32 to −0.03; back-transformed emotional exhaustion score=16.2; 95% CI, 14.7 to 17.3 vs. control score of 17.9). Organization-directed interventions showed a comparatively larger (moderate) reduction in burnout (SMD=−0.45; 95% CI, −0.62 to −0.28; back-transformed emotional exhaustion score=13.9; 95% CI, 12.4 to 14.7 vs. control score of 17.9).
The most effective interventions for reducing burnout combined structural changes, with communication between health care team members, and cultivated a sense of teamwork and job control. [13] However, these more complex organizational interventions were rare compared to simple reductions in workload or schedule changes. Future research should focus on whether different interventions work better for younger vs. more experienced physicians.
5) Genetic Testing and Counseling Among Patients With Newly Diagnosed Breast Cancer [14]
A study looking at women with newly diagnosed breast cancer, and, using a guideline-concordant measure of high pretest risk for mutation carriage, [15] found that only 52.9% of patients who were at high risk for germline mutations, i.e. BRCA 1 and 2, reported having genetic testing. Of those patients who underwent testing, 61.7% had a genetic counseling session. This highlights a missed opportunity to prevent ovarian and other cancer death among mutation carriers and their families as well as a gap between the need and availability of genetic counseling.
6) Quality of care delivered by general internists in US hospitals who graduated from foreign versus US medical schools: observational study [16]
Using a large database of Medicare patients, it was shown that elderly patients treated by graduates of international medical schools had a lower risk adjusted mortality compared with those treated by U.S. medical school graduates (adjusted mortality 11.1% v 11.7%; adjusted odds ratio 0.94, 95% confidence interval 0.92 to 0.95; P<0.001). While differences were modest, and there are several variables that need to be further explored, the data suggests the rigorous residency application process for international medical graduates selects for capable and experienced physicians.
7) Nicotine, Carcinogen, and Toxin Exposure in Long-Term E-Cigarette and Nicotine Replacement Therapy Users: A Cross-sectional Study [17]
This cross-sectional study evaluated the range of toxin levels measured in smokers and former smokers with or without concurrent long-term use of e-cigarettes or NRT using breath, saliva, and urinary samples. Patients using long-term e-cigarettes only or nicotine replacement therapy (NRT) only were found to have similar levels of nicotine compared to traditional combustible cigarettes, but with significantly reduced levels of measured carcinogen and toxins relative to smoking only combustible cigarettes.
Dr. Thatcher Heumann is a 1st year resident at NYU Langone Medical Center
Peer reviewed by Kevin Hauk, MD., attending physician. NYU Hospitalist Group, NYU Langone Medical Center
Image courtesy of Sports Illustration, http://cdn-s3.si.com/s3fs-public/2017/02/07/julian-edelman-sports-illustrated-super-bowl-cover.jpg
References
- Staff E. The insane number of records set or tied in Super Bowl LI. 2017. http://www.espn.com/blog/nflnation/post/_/id/230729/the-insane-number-of-records-set-or-tied-in-super-bowl-li
- Ataga KI, Kutlar A, Kanter J, Liles D, Cancado R, Friedrisch J, et al. Crizanlizumab for the Prevention of Pain Crises in Sickle Cell Disease. N Engl J Med. 2017;376(5):429-439. https://www.ncbi.nlm.nih.gov/pubmed/27959701
- Shipley WU, Seiferheld W, Lukka HR, Major PP, Heney NM, Grignon DJ, et al. Radiation with or without Antiandrogen Therapy in Recurrent Prostate Cancer. N Engl J Med. 2017;376(5):417-428. https://f1000.com/prime/727258259
- Bolla M, Gonzalez D, Warde P, Dubois JB, Mirimanoff RO, Storme G, et al. Improved survival in patients with locally advanced prostate cancer treated with radiotherapy and goserelin. N Engl J Med. 1997;337(5):295-300.
- Kinsinger LS, Anderson C, Kim J, Larson M, Chan SH, King HA, et al. Implementation of Lung Cancer Screening in the Veterans Health Administration. JAMA Intern Med. 2017. http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2599437
- National Lung Screening Trial Research T, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395-409.
- Moyer VA, Force USPST. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(5):330-338.
- Boiselle PM, Chiles C, Ravenel JG, White CS. Computed tomographic screening for lung cancer trends at leading academic medical centers from 2013 to 2015. JAMA Oncology. 2016;2(5):682-684.
- Panagioti M, Panagopoulou E, Bower P, Lewith G, Kontopantelis E, Chew-Graham C, et al. Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-analysis. JAMA Intern Med. 2017;177(2):195-205. https://www.research.manchester.ac.uk/portal/en/publications/a-systematic-review-and-metaanalysis-of-controlled-interventions-to-reduce-burnout-in-physicians(1b86a616-48a0-41a8-96bb-936367756cdb)/export.html
- Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, et al. Changes in Burnout and Satisfaction With Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613.
- Awa WL, Plaumann M, Walter U. Burnout prevention: a review of intervention programs. Patient Educ Couns. 2010;78(2):184-190.
- West CP, Dyrbye LN, Sloan JA, Shanafelt TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24(12):1318-1321.
- Linzer M, Poplau S, Grossman E, Varkey A, Yale S, Williams E, et al. A Cluster Randomized Trial of Interventions to Improve Work Conditions and Clinician Burnout in Primary Care: Results from the Healthy Work Place (HWP) Study. J Gen Intern Med. 2015;30(8):1105-1111.
- Kurian AW, Griffith KA, Hamilton AS, et al. Genetic testing and counseling among patients with newly diagnosed breast cancer. JAMA. 2017;317(5):531-534. http://jamanetwork.com/journals/jama/fullarticle/2600457
- Daly MB, Pilarski R, Axilbund JE, Berry M, Buys SS, Crawford B, et al. Genetic/Familial High-Risk Assessment: Breast and Ovarian, Version 2.2015. J Natl Compr Canc Netw. 2016;14(2):153-162.
- Tsugawa Y, Jena AB, Orav EJ, Jha AK. Quality of care delivered by general internists in US hospitals who graduated from foreign versus US medical schools: observational study. Bmj. 2017;356:j273.
- Shahab L, Goniewicz ML, Blount BC, Brown J, McNeill A, Alwis KU, et al. Nicotine, Carcinogen, and Toxin Exposure in Long-Term E-Cigarette and Nicotine Replacement Therapy Users: A Cross-sectional Study. Ann Intern Med. 2017.

One comment on “Primecuts – This Week in the Journals”
The juxtaposition of serious medical reviews concerning ultimate issues of human health and life with the ridiculously trite, a review of a commercial Football tournament (miraculous feat?), which is the is the current culture’s iteration of the Roman Circus puzzles me on this excellent blog.
Comments are closed.