Faculty Peer Reviewed
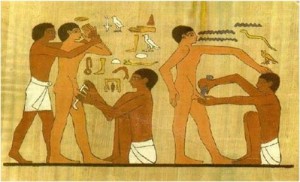
The earliest documented evidence of circumcision is in artwork from the Sixth Dynasty in Egypt (2345-2181 BC) found in a wall relief from Saqqara in Lower Egypt. Circumcised North Americans were described by Columbus upon arrival to the continent; circumcision was practiced by Australian aboriginals, native South Americans, and Pacific Islanders. It is unknown if circumcision was common amongst some earlier ancestor of all these peoples, or if it evolved independently in societies that lived in dry, sandy areas, where sand could get under the foreskin and lead to balanitis and urethritis. Throughout history, circumcision was often performed due to its perceived medical benefits, from curing excessive masturbation to decreasing rates of infection, but the practice fell out of favor in the last century within the medical community as there was insufficient data to support these claims. Today, reasons for circumcision often stem from religious beliefs or social customs, but now there is some compelling data showing that circumcision may be beneficial to one’s health.
Sub-Saharan Africa remains the region most heavily affected by HIV. In 2008, it accounted for 67% of HIV infections worldwide, 68% of new HIV infections among adults and 91% of new HIV infections among children. The region also accounted for 72% of the world’s AIDS-related deaths. A link between circumcision rates and HIV prevalence in heterosexual men in Africa was first hypothesized in the late 1980s, when researchers studying risk factors for HIV infection in 422 men who visited commercial sex workers found that men who were not circumcised had an 8.2 fold increased risk of seroconversion compared with circumcised men.[3] Additional studies found similar (though not as striking) trends, and a meta-analysis showed an adjusted relative risk of 0.42. In further support of their theory, a cohort study of Ugandan discordant couples in which the female was HIV infected and the male partner was initially HIV seronegative, 37 of 134 uncircumcised men while none of 50 circumcised men became seropositive after approximately 2 years of follow-up. [11] When one looks at a map of AIDS prevalence in the 1990s, one can see a distinct area of overlap: The areas of high prevalence (also known as the “AIDS beltâ€) coincide with areas where circumcision rates are lower than other parts of Africa. The researchers looked into a variety of confounders such as prostitution, IVDU and homosexuality and were still able to show association.
“Orange Farm†was the first randomized, controlled, blindly evaluated trial to look at male circumcision as an intervention to prevent acquiring HIV. The primary objective of the trial was to determine the impact that male circumcision would have on the acquisition of HIV by young men. A total of 3274 uncircumcised men, aged 18 to 24, were randomized to a control or an intervention group with follow-up visits at months 3, 12 and 21. Circumcision was offered to the intervention group immediately and to the control group at the end of the study. The trial was stopped at the interim analysis (mean follow-up: 18.1 months), when analysis showed a risk ratio of 0.42 with 20 HIV infections in the intervention group and 49 infections in the control group, signifying an approximate protection rate of 60% with the intervention of male circumcision. [1] Subsequent trials in Kisumu, Kenya and Rakai, Uganda showed risk ratios of 0.41 and 0.50 respectively; these trials were also stopped during their interim analysis. [2, 5] The pooled analysis shows that in a two year period, in order to prevent one HIV infection, approximately 72 circumcisions will have to be performed. [7]
As a means to explain the results of all three trials, one must consider the following: The presence of penile foreskin makes for a larger total surface area over which the HIV virus can invade, and the area under the foreskin is warm and moist which is a favorable environment for pathogen survival and replication. With a foreskin in place, there is a longer drying time after sexual contact, which increases life expectancy of HIV on the penis after sexual activity. The inner surface of the foreskin is not keratinized, making it prone to micro tears during sex. Of more probable importance, there are a larger number of target cells for HIV in the foreskin in comparison to keratinized penile skin (nine times the number of target cells; including Langerhaans cells, CD4+ T cells, and macrophages). [8] Â It is important to note that a retrospective study looking at the control group of men who seroconverted in the Rakai study, at the two year mark when the control groups were also circumcised, found that the men who seroconverted had on average possessed larger foreskin areas than the members of the study who remained HIV negative. [6]
The current recommendations regarding male circumcision are still under discussion, but there now exists mounting data to support male circumcision as primary protection against female-to-male acquisition of HIV during vaginal intercourse. UNAIDS/WHO met in 2007 to discuss the trials, and recommended that it is important to stress the fact that male circumcision will never provide complete protection from HIV, but that it may be a good adjunct to condom use in areas where heterosexual HIV transmission rates are high and men are not commonly circumcised. Â [12]
Researchers also looked at male-to-female transmission of HIV, but the results were not conclusive. 922 uncircumcised, HIV-infected, asymptomatic men aged 15-49 with CD4 counts 350 or more were enrolled in an unblinded, randomized controlled trial in Rakai District in Uganda. The intervention group was circumcised immediately, and HIV-uninfected female partners of these men were concurrently enrolled. 18% of women in the intervention group and 12% in the control group became infected but the results were deemed statistically insignificant. There was a subanalysis, not specified in the protocol, which looked at HIV transmission rates in couples who had had early resumption of sexual relations after circumcision prior to complete healing. Five out of eighteen women in the intervention group who had early resumption of sex became HIV positive (27.8%) with a rate ratio of 3.5 (p value 0.038), and in the intervention group who waited until after healing to resume sexual activity, 6 out of 63 women became HIV positive.  Of the control group composed of uncircumcised HIV-infected men with uninfected female partners, 5 out of 63 women seroconverted.[10]  Needless to say, it stands to reason that early resumption of sexual activity would increase male to female transmission in the setting of continued penile wound healing. HIV-positive men undergoing circumcision should receive extensive counseling regarding the increased risk of infection they pose to their partners during the period of healing. Studies looking at the spread of other sexually transmitted infections in circumcised versus uncircumcised men are as yet inconclusive. [9]
This data might not be applicable to the US where the population and its sexual practices differ from those in sub-Saharan Africa. According to the CDC, which compiles data from the 34 states that have confidential name-based HIV infection reporting, male-to-male sexual activity accounted for 62% of all reported sexually transmitted cases of HIV in 2007. Of the reported cases of heterosexual transmission, approximately 65% were male to female; meaning that about 13% of HIV transmission in the US was female to male heterosexual transmission. The studies reviewed in this article look only at female to male transmission in populations with low rates of circumcision. The fact that these trials may not affect policy in the US, is likely the reason why there has been limited local publicity surrounding the data. Despite the lack of local news coverage, these studies are of enormous importance as widespread implementation of circumcision in countries with low prevalence of male circumcision and high rates of heterosexual transmission should help to curb the spread of HIV.
Dr. Taylor is an Attending Physician, Dept. of Medicine, NYU Langone Trinity Center
Peer reviewed by Melanie Maslow, Â MD, Â Section Editor, Infectious Diseases, Clinical Correlations
References:
1. Auver B et al. Randomized, Controlled Intervention Trial of Male Circumcision for Reduction of HIV Infection Risk: The ARNS 1265 Trial. PLoS Medicine 2005; 2: 1112-21.
2. Bailey RC et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet 2007; 369: 643-56. http://www.ncbi.nlm.nih.gov/pubmed/17321310
3. Cameron DW,et al. Female to male transmission of human immunodeficiency virus type 1: risk factors for seroconversion in men. Lancet 1989; 2: 403-7. http://www.ncbi.nlm.nih.gov/pubmed/2569597
4. Drain PK et al. Male circumcision, religion, and infectious diseases: an ecologic analysis of 118 developing countries. BMC Infectious Diseases 2006; 6: 172. http://www.biomedcentral.com/1471-2334/6/172
5. Gray RH et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet 2007; 369: 657-65.
6. Kigozi G et al. Foreskin surface area and HIV acquisition in Rakai, Uganda (size matters). AIDS 2009; 23: 2209-13.
7. Mills E et al. Male circumcision for the prevention of heterosexually acquired HIV infection: a meta-analysis of randomized trials involving 11 050 men. HIV Medicine 2008; 9: 332-5. http://www.ncbi.nlm.nih.gov/pubmed/18705758
8. Szabo R et al. How does male circumcision protect against HIV infection? BMJ 2000; 320: 1592-4
9. Tobian AAR et al. Male Circumcision for the Prevention of HSV-2 and HPV infections and Syphilis. NEJM 2009; 360: 1298-309. http://www.nejm.org/doi/full/10.1056/NEJMoa0802556
10. Wawer MJ et al. Circumcision in HIV-infected men and its effect on HIV transmission to female partners in Rakai, Uganda: a randomised controlled trial. The Lancet 2009; 374: 229-37. http://www.hivinsite.org/InSite?page=jl-56-03
11. Weiss HA et al. Male circumcision and risk of HIV infection in sub-Saharan Africa: A systematic review and meta-analysis. AIDS 2000; 14: 2361-70. http://www.circs.org/library/weiss/index.html
12. WHO/UNAIDS. WHO and UNAIDS announce recommendations from expert meeting on male circumcision for HIV prevention. http://data.unaids.org/pub/PressRelease/ 207/20070328_pr_mc_recommendations_en.pdf