 Commentary by Melissa Freeman MD, PGY2
Commentary by Melissa Freeman MD, PGY2
Modern day science has revealed to us the intricate relationships that thyroid hormones have with multiple systems of the human body. Many of today’s physicians find themselves checking patients’ thyroid function tests (TFTs) almost as reflexively as a baseline basic metabolic panel. Yet, what seems to the physician to be a harmless bit of thoroughness can often turn into hours of inquisitive head scratching if the TFTs reveal subclinical thyroid dysfunction, especially since automated assays for TFTs are more sensitive than ever.
The ingredients to make a diagnosis of subclinical thyroid dysfunction include an abnormal serum thyroid-stimulating hormone (TSH) combined with serum thyroid hormone levels that are within normal reference range. At present, the treatment of overt thyroid dysfunction is largely straightforward. However, the evidence for treating subclinical thyroid dysfunction is controversial, making way for varying expert opinion. What follows is a brief, selective look at some of the issues surrounding the treatment of subclinical thyroid dysfunction; it is by no means inclusive. This topic will be presented as a two-part installment; Part I will review definitions and consequences of subclinical thyroid dysfunction and Part II will focus on treatment recommendations and conclusions.
Subclinical hyperthyroidism is defined as a decreased serum TSH level with normal levels of free T4 and free T3. Though reports vary significantly based on diet and geography, the estimated prevalence of subclinical hyperthyroidism is roughly 2%. Women, elderly, and blacks however appear to be at increased risk. It can be classified as either exogenous, secondary to the ingestion of thyroid hormone, or endogenous, secondary to entities such as Graves’ disease, toxic multinodular goiter, thyroiditis, or autonomously functioning solitary nodules. Exogenous subclinical hyperthyroidism can actually be a goal of thyroid hormone therapy in a patient with a history of cancer requiring suppression. One must also consider early central hyperthyroidism, pregnancy, critical illness, and even normal variations with aging in the differential of an isolated low serum TSH. Still, the most common reason for an isolated low TSH is recent hypothyroidism, with a lag in TSH response to normalcy.
Studies of the clinical significance of endogenous subclinical hyperthyroidism note adverse consequences such as an increased risk of cardiovascular mortality, diastolic dysfunction, tachycardia, left ventricular hypertrophy, atrial fibrillation, and anxiety. It is also reported that in post-menopausal women with subclinical hyperthyroidism, bone mineral density at all sites is lower than those in comparable euthyroid populations. Increased fracture risk has been associated with this patient population as well. The effects of therapy on the above pathologies have been minimally studied and the conclusions are quite variable; some studies show improved end points after treatment in these patients, while others are without any treatment effect. In order to support or refute treatment urgency, researchers have focused on studying the reversion and progression rates of subclinical hyperthyroidism. For example, in a one year cohort study, Parle et al. (1991) found that in patients with TSH values between 0.05 and 0.5 mU/liter, TSH values reverted to normal in 38 of 50 patients, but remained unchanged in 14 of 16 patients with a baseline TSH less than 0.05 mU/L. Sawin et al. (1991) followed an elderly population with TSH levels less than 0.1 mU/liter over a 4 year period and found a 4.1% rate of progression to hyperthyroidism in these patients. Still, the above studies must be looked at critically as they are small studies with narrowed populations.
Subclinical hypothyroidism, also known as compensated hypothyroidism, preclinical hypothyroidism, or mild thyroid failure, is defined as an elevated serum TSH level with a normal serum free T4. It is believed to be more common than subclinical hyperthyroidism with an estimated, notably variable, prevalence of 4-10%, greatest in elderly females. Causes include chronic autoimmune thyroiditis, prior ablative therapy, and inadequate T4 replacement therapy.
Current literature suggests that the adverse consequences of subclinical hypothyroidism include diastolic dysfunction, cardiovascular disease, lipid abnormalities (increased total and LDL levels), and neuropsychiatric symptoms. A fair amount of attention has been focused on the effect of subclinical hypothyroidism on the cognitive functioning and mood of the elderly population. Understanding that overt hypothyroidism can slow cognitive function and dampen mood in this demographic, researchers wonder if “a little bit†of hypothyroidism has a similar, but graded, effect. Though studies are somewhat split in their findings on this topic, the larger and better-designed studies seem to refute an association between subclinical hypothyroidism, cognition, and mood. A recent cross-sectional study by Lesley et. al. (2006) sought to determine a specific association between subclinical thyroid dysfunction and cognition, depression, and anxiety in a population of 5,865 patients over 65 years of age. After TFTs were obtained, patients were analyzed via the Hospital Anxiety and Depression Scale, the Middlesex Elderly Assessment of Mental State Examination, and the Folstein Mini-Mental Status Examination. After controlling for confounding variables, no association was found between subclinical hypothyroidism and cognitive or mood disorders.
Logically, if both subclinical hyperthyroidism and hypothyroidism are linked, whether weakly or strongly, to adverse outcomes, it seems only right to treat patients with this condition. Yet, how are we to digest the conflicting studies and possibility that it may just revert back to normal? What about the risks and drawbacks of taking a potentially unnecessary medication? Stay tuned for the next blog installment of “Subclinical Thyroid Dysfunction,†which will discuss the current recommendations on the treatment of subclinical thyroid disease.
References:
Caraccio, N., Ferrannini, E, Monzani, F. Lipoprotein profile in subclinical hypothyroidism: response to levothyroxine replacement; a randomized controlled study. J Clin Endocrinol Metab. 2002; 87: 1533-1538.
Cooper, David S.. Approach to the patient with subclinical hyperthyroidism. J Clin Endocrinol and Metab. 2007; 92(1): 3-9.
Hossein, G. R., Tuttle, M. H., Baskin, J., Fish, L., Singer, P., McDermott, M. T. . Consensus Statement: A Joint Statement on Management from the American Association of Clinical Endocrinologists, the American Thyroid Association, and the Endocrine Society. J Clin Endocrinol and Metab. 2005; 90(1): 581-585.
Parle JV, Franklyn JA, Cross KW, Jone SC, Sheppard MC. Prevalence and follow-up of abnormal thyrotropin concentrations in the elderly in the United Kingdom. J Clin Endocrinol. 1991 34: 77-83.
Roberts, L.M., Pattison, H., Roalfe, A., Franklyn,J., Wilson, S., Hobbs, R., Parle, J. V.. Is subclinical thyroid dysfunction in the elderly associated with depression or cognitive dysfunction? Annals of Intern Med, 2006; 145: 573-581.
Ross, D. “Subclinical hypothyroidism,†“Subclinical hyperthyroidism†@UpToDate.com, accessed 6/28/07, 12:40pm.
Sawin CT, Geller A., Kaplan MM, Bacharch P, Wilson PW, Hershman JM. Low serum thyrotropin concentrations in older persons without hyperthyroidism. Arch Intern Med. 1991; 151: 165-168.
Wartofsky, L., Dickey, R. A. The evidence for a narrower thyrotropin reference range is compelling. J Clin Endocrin and Metab. 2005; 90(9): 5483-5488.
Wilson, S., Parle, J., Roberts, L, Roalfe, A. Hobbs, R., Clark, P., Sheppard, M., Gammage M., Pattison, H., Jayne, A. F. Prevalence of subclinical thyroid dysfunction and its relationship to socioeconomic deprivation in the elderly: a community-based cross-sectional survey. J Clin Endocrin and Metab. 2006; 91(12): 4809-4816.
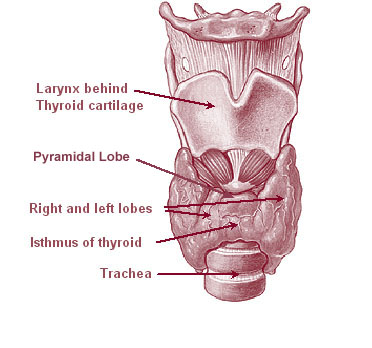
Image courtesy of Wikimedia Commons

One comment on “Part I- Subclinical Thyroid Dysfunction: To Treat or Not to Treat?”
Comments are closed.