Faculty Peer Reviewed
CASE: A 54-year-old Asian female with no significant past medical history presents to her primary care physician with the complaint of several weeks of pain in her fingers bilaterally along with pronounced, worsening morning stiffness. She is subsequently diagnosed with rheumatoid arthritis (RA), and the decision is made to start her on long-term, high-dose non-steroidal anti-inflammatory drugs (NSAIDs). Given the link between NSAIDs and peptic ulcer disease (PUD), should this patient first be tested, and if positive, treated for Helicobacter pylori (H. pylori)?
It has been widely recognized that infection with H. pylori predisposes individuals to PUD as well as gastric adenocarcinoma and gastric mucosa-associated lymphoid tissue (MALT) lymphoma. Though the effect of eradication of H. pylori on the development of gastric carcinoma remains unclear [1], it has been well-established that elimination of H. pylori significantly reduces the risk of development of PUD. As effective non-invasive means for diagnosis of H. pylori exist(urea breath test, serological tests, and stool antigen assays), along with effective means for treatment, the question of when and who to treat arises.
One specific group of individuals for whom this question has been raised is those patients requiring chronic treatment with NSAIDs, a large-percentage of whom have RA. NSAIDs are wellestablished risk factors for the development of both uncomplicated and complicated PUD [2]. In those individuals with rheumatologic diseases, NSAID-induced PUD is a frequently-encountered issue, with the incidence being reported as high as 1.2-1.6% per year in patients with RA [3].
Overall, it has been estimated that H. pylori, NSAIDs, or a combination of the two account for 90-95% of gastric and duodenal ulcers [4]. Though studies have historically reported conflicting data regarding the effect of H. pylori infection on PUD development in chronic NSAID users, a meta-analysis performed by Huang, et al. in 2002 showed that NSAID users infected with H. pylori are 3.5 times as likely to develop PUD than those that were not infected [5]. Therefore, the eradication of H. pylori in individuals prior to the onset of chronic NSAID use seems to be a logical step in reducing the likelihood of PUD in those individuals.
Epidemiologic studies have shown that the most substantial increase in incidence of PUD during NSAID treatment occurs during the initial 3 months of treatment [6]. This is likely due to the fact that the initiation of NSAIDs aggravates PUD in patients that are already susceptible to the disease. Therefore, patients are likely to benefit most from H. pylori eradication prior to NSAID treatment induction rather than after NSAID treatment has been initiated.
Multiple studies have been undertaken to investigate the development of PUD in chronic NSAID users who have undergone H. pylori eradication versus those that have not. In a meta-analysis by Vergara, et al. in 2005 encompassing the most influential randomized, controlled studies to date, it was shown that all of the studies found a significant difference or a positive trend in favor of eradication therapy [7]. The odds-ratios for the prevention of PUD in the eradication groups ranged from 0.2-0.82 in the 4 studies included in the final analysis with a combined OR of 0.43. The range for number needed to treat(NNT) was 4.8-70, and the NNT when all studies were combined was 16.9. The studies were further analyzed in subgroups of NSAID-naïve patients versus those already undergoing long-term NSAID therapy. This analysis revealed a large discrepancy in ulcer development following H. pylori eradication. In the NSAID-naïve group, there was a significant OR of 0.26 (13.7% in non-eradicated vs. 3.8% in eradicated), while in the group already undergoing chronic NSAID therapy, there was a non-significant OR of 0.95 (12.8% in non-eradicated vs. 12.1% in eradicated). This suggests that H. pylori eradication in patients already undergoing NSAID therapy may not be beneficial for the reduction of ulcer development.
Importantly, in a study by Chan, et al. in 2001, it was shown that H. pylori eradication in and of itself is not sufficient to protect chronic NSAID users with recent ulcer complications from further GI events [8], though the addition of long-term PPI treatment does result in a significant reduction of recurrent bleeding. Similar findings were reported by Hawkey, et al. in their 1998 study [9].
Therefore, based on the currently available data, it is this author’s suggestion that all patients should undergo H. pylori testing (and treatment, if positive) prior to the initiation of long-term NSAID treatment. Furthermore, in patients with a history of bleeding ulcer, long-term PPI therapy in addition to H. pylori eradication is recommended. In contrast, it is not recommended to diagnose and treat H. pylori in patients who have already undergone NSAID treatment as it does not appear to significantly decrease the rate of ulcer development.
Dr. Smith is a first year resident at NYU Langone Medical Center
Peer reviewed by Michael Poles, MD, Section Editor, GI, Clinical Correlations
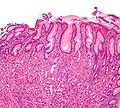
Image courtesy of Wikimedia Commons (Description 1 High magnification micrograph of gastritis with Helicobacter pylori ).
References
1. Wong BC, Lam SKL, Wong WM, et al. Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China. J Am Med Assoc 2004;291:187–94.
2. Chan FKL, Leung WK. Peptic-ulcer disease. Lancet 2002;360:933–41.
3. Fries JF, Murtagh KN, Bennett M, Zatarain E, Lingala B, Bruce B. The rise and decline of nonsteroidal antiinflammatory drug-associated gastropathy in rheumatoid arthritis. Arthritis Rheum 2004;50:2433–40. http://onlinelibrary.wiley.com/doi/10.1002/art.20440/full
4. Kurata JH, Nogawa AN. Meta-analysis of risk factors for peptic ulcer. Nonsteroidal anti-inflammatory drugs, Helicobacter pylori, and smoking. J Clin Gastroenterol 1997;24:2-17.
5.  Huang JQ, Sridhar S, Hunt RH. Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: a meta-analysis. Lancet 2002;359:14–22. http://www.ncbi.nlm.nih.gov/pubmed/11809181
6.  Langman MJ, Weil J, Wainwright P, et al. Risks of bleeding peptic ulcer associated with individual non-steroidal anti-inflammatory drugs. Lancet 1994;343:1075–8. http://www.ncbi.nlm.nih.gov/pubmed/7909103
7.  Vergara M, Catalan M, Gisbert JP, Calvet X. Meta-analysis: role of Helicobacter pylori eradication in the prevention of peptic ulcer in NSAID users. Aliment Pharmacol Ther 2005;21:1411–8. http://www.ncbi.nlm.nih.gov/pubmed/15948807
8. Chan FKL, Chung SCS, Suen BY, et al. Preventing recurrent upper gastrointestinal bleeding in patients with Helicobacter pylori infection who are taking low-dose aspirin or naproxen. N Engl J Med 2001;344:967–73. http://www.nejm.org/doi/full/10.1056/NEJM200103293441304
9.  Hawkey CJ, Tulassay Z, Szczepanski L, et al. Randomised controlled trial of Helicobacter pylori eradication in patients on non-steroidal anti-inflammatory drugs: HELP NSAIDs study. Lancet 1998;352:1016–21.