Faculty Peer Reviewed
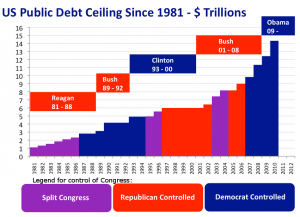
Talks between President Obama and House Republicans were described as “cordial but fruitless,†as they again failed to reach an agreement on a six-week extension of the nation’s borrowing authority over the holiday weekend. As elected officials try to sway public opinion on which party bears responsibility for the shutdown, and salvage the greater portion of the 5% approval rating currently enjoyed by Congress, the roll out of Obamacare begins slowly but visibly in the community. Despite the nuisance of insurance company representatives peddling their premiums outside our hospitals, it’s business as usual for patients, hospital staff, and housestaff on the Medicare payroll. In hope that something positive will emerge from the ashes of partisanship and negativity in Washington, this week’s Primecuts highlights some important contributions negative trials have made to the medical literature.
This week, the New England Journal of Medicine published the Cardiac-Resynchronization Therapy in Heart Failure with a Narrow QRS Complex trial, which was an international, multicenter, randomized trial designed to evaluate cardiac resynchronization therapy (CRT) in patients with chronic systolic heart failure and a narrow QRS complex [1].
Current guidelines do not recommend CRT for patients with normal QRS duration regardless of the presence of mechanical dyssynchrony, This trial examined patients with New York Heart Association (NYHA) class III or IV heart failure with a left ventricular ejection fraction of 35% or less, a standard indication for an implantable cardioverter-defibrillator (ICD), and a QRS duration of less than 130msec with echocardiographic evidence of left ventricular dyssynchrony. The primary efficacy outcome was the combination of death from any cause or first hospitalization for worsening heart failure.
The study was stopped early for futility on the recommendation of the data and safety monitoring board when it was found that the hospitalization rate for worsening heart failure did not differ significantly between the two groups, (hazard ratio [HR] 1.11, 95% confidence interval [CI] 0.88 to 1.4). However in the CRT group, 45 of 404 patients (11.1%) died, 37 from cardiovascular causes, as compared with 26 of 405 (6.4%) in the control group, with only 17 from cardiovascular causes (HR 1.81; 95% CI 1.11 to 2.93). As a result, widened QRS remains the primary determinant of the response to CRT; with echocardiographic evidence of dyssynchrony not predictive of benefit.
In other screening news, we all know that many people who could benefit are not screened for colorectal cancer (CRC). What you may not know is that the recommendation of a primary care physician (PCP) is one of the strongest predictors of adherence to CRC screening [2,3]. This week, the Annals of Internal Medicine published a large, population-based case-control study entitled Primary Care Utilization and Colorectal Cancer Incidence and Mortality Among Medicare Beneficiaries, which examined the association of primary care utilization with CRC incidence, CRC deaths, and all-cause mortality [4]. The study looked at persons aged 67 to 85 years diagnosed with CRC between 1994 and 2005 in U.S. Surveillance, Epidemiology, and End Results (SEER) regions matched with control patients (n = 205,804 for CRC incidence, 54,160 for CRC mortality, and 121,070 for all-cause mortality). Primary care visits were measured in the 4- to 27-month period before CRC diagnosis, CRC incidence, CRC mortality, and all-cause mortality. Compared with persons having 0 or 1 primary care visit, persons with 5 to 10 visits had lower CRC incidence (adjusted odds ratio [OR] 0.94; 95% CI 0.91 to 0.96) and mortality (adjusted OR 0.78; 95% CI 0.75 to 0.82) and lower all-cause mortality (adjusted OR 0.79; CI 0.76 to 0.82), mediated by ever receipt of CRC screening and polypectomy. This observational study found that people enrolled in Medicare who had more primary care visits were less likely to develop or die from colorectal cancer and had a lower mortality from all causes combined. Although this study’s observational design prevents a causal analysis, the use of a comparison group improves upon a previous cohort study of Medicare beneficiaries with CRC by eliminating lead-time bias [4].
The conundrum of comparison groups was also addressed by the British Medical Journal this week in a meta-epidemiological study of the comparative effectiveness of exercise and drug interventions on mortality outcomes [5]. This study showed that a structured exercise program may be as good as, or better than frequently prescribed drugs for some common cardiovascular ailments; however, the comparison of exercise and drug interventions was tempered by differences in patient populations across different trials, the scarcity of data, and the different settings involved. Despite these limitations, this meta-epidemiological review is the first to compare the mortality benefits of exercise and drug interventions. Given the scarcity of financial resources (and incentives) to fund future trials of exercise interventions, authors suggest requiring pharmaceutical sponsors of new drugs to include exercise interventions as an active comparator arm in drug trials for market entry, an idea regulators should consider running with.
Noninferiority trials are common in medical literature. This week the New England Journal of Medicine published a study of Edoxaban (an oral factor Xa inhibitor) versus Warfarin for the Treatment of Symptomatic Venous Thromboembolism [6]. In this randomized, double-blind, noninferiority study, patients with acute venous thromboembolism (VTE), who had initially received heparin, were randomized to receive edoxaban or warfarin. In the primary efficacy outcome of recurrent symptomatic venous thromboembolism, edoxaban was shown to be noninferior to warfarin, with a hazard ratio of 0.89 (95% CI 0.70 to 1.13; P<0.001 for noninferiority) with less major or clinically relevant nonmajor bleeding, providing another viable alternative to INR checks for patients with symptomatic VTE.
Other noteworthy articles this week include:
In JAMA, Papazian et. al looked at the effect of statin therapy on mortality in patients with Ventilator Associated Pneumonia (VAP) [7]. Although this trial was terminated early when interim analysis showed higher mortality in the group of VAP patients treated with adjunctive simvastatin, its randomized controlled design provides a significant departure from the observational designs limiting previous research on the anti-inflammatory and immunomodulating effects of statins in sepsis.
In research of potential therapies slightly farther down the pipeline, and phylum, original research demonstrates a peptide isolated from Chinese red-headed centipede (Scolopendra subspinipes mutilans) venom is as potent as morphine at treating pain [8]. In vivo, mice injected with the molecule show less response to painful stimuli (exposure to noxious chemicals or heat) with no obvious side effects, suggesting that this molecule, and perhaps others, could yield powerful new treatments for pain.
In Gastroenterology this week, a study by Gawrieh et al used noninvasive tools to predict long-term hepatic and extrahepatic adverse outcomes in nonalcoholic fatty liver disease (NAFLD) [9]. This study was able to show a progressive increase in overall mortality rate with increasing fibrosis scores after adjustment for other known predictors of mortality, providing a noninvasive means to risk stratify patients with NAFLD. Interestingly, almost all of the increased mortality risk was owing to cardiovascular causes.
Finally, an editorial in NEJM this week suggests ways to train future physicians to manage obesity including basic science foundations, training in behaviorism, and collaborative interdisciplinary care teams [10].
Dr. Kerrilynn Carney is a 1st year resident at NYU Langone Medical Center
Peer reviewed by Matthew Vorsanger, MD, Associate Editor, Clinical Correlations
Image courtesy of Wikimedia Commons
References:
1. Ruschitzka et al. Cardiac-Resynchronization Therapy in Heart Failure with a Narrow QRS Complex. N Engl J Med. 2013 Oct 10;369(15):1395-1405. Epub 2013 Sep 2. http://www.nejm.org/doi/full/10.1056/NEJMoa1306687
2. Klabunde et al. Barriers to colorectal cancer screening among Medicare consumers. Am J Prev Med 2006;30:313-319. http://www.ajpmonline.org/article/S0749-3797%2805%2900502-7/abstract
3. Wee et al. Factors associated with colon cancer screening: the role of patient factors and physician counseling. Prev Med 2005;41:23-29. http://www.sciencedirect.com/science/article/pii/S0091743504005729
4. Ferrante et al. Primary care utilization and colorectal cancer outcomes among Medicare beneficiaries. Arch Intern Med 2011;171:1747-1757. http://archinte.jamanetwork.com/article.aspx?articleid=1105994
5. Naci et al. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ 2013;347. http://www.bmj.com/content/347/bmj.f5577
6. The Hosukai-VTE Investigators. Edoxaban versus Warfarin for the Treatment of Symptomatic Venous Thromboembolism. New England Journal of Medicine 2013;369:1406-1415. http://www.nejm.org/doi/full/10.1056/NEJMoa1306638
7. Papazian et al. Effect of statin therapy on mortality in patients with ventilator-associated pneumonia: A randomized clinical trial. JAMA. 2013 Oct 9. http://jama.jamanetwork.com/article.aspx?articleID=1752244
8. Yang et al. Discovery of a selective NaV1.7 inhibitor from centipede venom with analgesic efficacy exceeding morphine in rodent pain models. Proc Natl Acad Sci U S A. 2013 Sep 30. http://www.pnas.org/content/early/2013/09/25/1306285110.long
9. Gawrieh et al. NAFLD Fibrosis Score: Is It Ready for Wider Use in Clinical Practice and for Clinical Trials? Gastroenterology 2013;145:717-719. http://www.gastrojournal.org/article/S0016-5085%2813%2901218-3/fulltext
10. Colbert et al. Training Physicians to Manage Obesity — Back to the Drawing Board. New England Journal of Medicine 2013;369:1389-1391. http://www.nejm.org/doi/full/10.1056/NEJMp1306460