Peer Reviewed
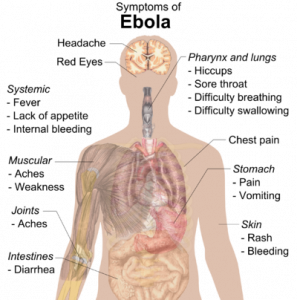
This week, the Ebola virus outbreak continues to dominate the news both here and abroad. The number of newly-diagnosed patients in West Africa continues to rise, particularly in Guinea, Liberia, and Sierra Leone, while Nigeria and Senegal have gone nearly four weeks without any new cases. International aid workers infected with Ebola continue to be transported out of affected areas back to their home countries, however as a consequence of this, new cases are now starting to arise outside of Africa among people caring for these patients. Here in the US, the first travel-associated case of Ebola was diagnosed in Dallas on September 30, and the patient unfortunately passed away eight days later. In the week since, two nurses involved in the care of this index patient have become infected. Despite efforts by hospitals and health departments around the country to demonstrate their preparedness, fear continues to spread among the public, especially given the recent WHO estimate that there could be 10,000 new cases per week in the upcoming months, which is ten times the current weekly rate of new cases. This is all of particular concern to those of us at Bellevue Hospital, which is the designated Ebola center for all of New York City.
Given the extent of public concern regarding the outbreak of Ebola, it should be no surprise that there is a great deal being written about the deadly virus in the medical literature. Just this week, the New England Journal of Medicine published an overview of the epidemic as well as future projections, as authored by the WHO Ebola Response Team[1]. This article details that the majority of those infected in West Africa are between the ages of 15-44, that about 50% are male, and that the case fatality rate is 70.8%. The authors estimated the average incubation period is 11.4 days, and project that the cumulative total number of cases in West Africa, assuming no major changes in the current disease course, will exceed 20,000 by November 2, 2014. Interestingly, another article on Ebola was published online by the same journal just the day before, this one regarding the outbreak of a different strain of Ebola virus in the Democratic Republic of Congo[2].
Moving on from Ebola, a large study looking at long-term outcomes in patients with symptomatic carotid artery stenosis treated with stenting versus surgery was published in The Lancet this week[3]. The study, ICSS (International Carotid Stenting Study), was a large, international, 50-center trial which randomly assigned patients with symptomatic carotid stenosis to treatment with either carotid artery stent placement versus carotid endarterectomy. Major outcomes were assessed by an independent committee and the primary endpoint was fatal or disabling stroke at any point during follow-up, the median of which was 4.2 years. Analysis was done via intention-to-treat, and the results showed that there was no significant difference in the primary endpoint between the two groups. This goes against current thinking that endarterectomy is the preferred treatment for carotid stenosis for patients with symptomatic carotid stenosis and standard surgical risk, and may actually end up changing management.
Another study, published recently in Circulation, sought to determine if intensive endurance training could lead to beneficial structural remodeling of the heart, as seen in elite athletes[4]. This study included 12 previously sedentary individuals (seven men, five women, ages 23-35) who underwent an increasingly intense physical conditioning regimen such that they would be fit to compete in a marathon. Cardiac MRI was done prior to beginning the regimen and then at 3-month intervals over the course of one year to chart any changes in left and right ventricular volume and mass. They also measured maximum oxygen uptake and cardiac output at the same times, and pulmonary artery catheterization was performed prior to starting the regimen as well as after completing it at one year. Pressure/volume and Starling curves were also constructed and compared to those of elite athletes.
The results demonstrated that LV and RV mass increased progressively throughout the year and approximated levels of elite athletes. RV volume also progressively increased, however LV volume did not significantly change until after six months of training. The authors concluded that even only after one year, such a training regimen can lead to morphologic changes in cardiac structure similar to those seen in the hearts of elite athletes, even in previously sedentary individuals.
The results of a study from our own institution was published this month in the Annals of Internal Medicine[5]. Drs. Joseph Ladapo and Saul Blecker studied how frequently physicians decide to order cardiac stress tests, particularly with imaging, due to the increasing emphasis being placed on reducing healthcare cost and waste, and improving value. The authors analyzed cross-sectional data collected via two national surveys administered to outpatient providers from 1993 to 2010 to determine how frequently stress tests were ordered, with special attention paid to demographics such as race and ethnicity to see if any disparities exist. The authors found that, from 1993-1995 and 2008-2010, the number of visits at which a stress test was ordered increased from 28 per 10,000 visits to 45, and that stress tests with imaging made up a growing portion of all stress tests ordered. They determined that of these, at least 34.6% were inappropriate, using appropriateness criteria put forth by several medical societies including the American College of Cardiology, the American Society of Nuclear Cardiology, and the American Society of Echocardiography. These inappropriate tests were associated with an estimated annual cost of $501 million and 491 future cases of cancer. The authors also determined that there was no disparity between blacks and whites in terms of ordering, and although there was a suggestion of such a disparity between whites and Hispanics, this difference did not reach statistical significance.
Other articles of note:
Cudkowicz et al. published a study evaluating if therapy with ceftriaxone can help patients with amyotrophic lateral sclerosis by modulating the expression of glutamate excitotoxicity[6].
In a new study published in JAMA this week, Kalil et al. investigated whether the vancomycin minimum inhibitory concentration (MIC) of Staphylococcus aureus in the setting of bloodstream infection has any effect on mortality[7].
Stacy et al. delve into the common clinical dilemma of a positive troponin in a patient with chronic kidney disease in a new study published this week in the Annals of Internal Medicine[8].
Dr. Anish Parikh is a 3rd year resident at NYU Langone Medical Center
Peer reviewed by Mark H. Adelman, MD, Associate Editor, Clinical Correlations
Image courtesy of Wikimedia Commons
References
1) WHO Ebola Response Team. Ebola Virus Disease in West Africa- The First 9 Months of the Epidemic and Forward Projections. N Engl J Med. 2014; 371:1481-1495. http://www.nejm.org/doi/full/10.1056/NEJMoa1411100
2) Maganga GD, Kapetshi J, Berthet N, et al. Ebola Virus Disease in the Democratic Republic of Congo. N Engl J Med. Published online 10/15/2014. http://www.nejm.org/doi/full/10.1056/NEJMoa1411099
3) Bonati LH, Dobson J, Featherstone RL, et al. Long-term outcomes after stenting versus endarterectomy for treatment of symptomatic carotid stenosis: the International Carotid Stenting Study (ICSS) randomised trial. Lancet. Published online 10/14/2014. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2814%2961184-3/fulltext.
4) Arbab-Zadeh A, Perhonen M, Howden E, et al. Cardiac Remodeling in Response to 1 Year of Intensive Endurance Training. Circulation. Published online 10/3/2014. http://circ.ahajournals.org/content/early/2014/10/03/CIRCULATIONAHA.114.010775.abstract
5) Ladapo JA, Blecker S, Douglas PS. Physician Decision Making and Trends in the Use of Cardiac Stress Testing in the United States: An Analysis of Repeated Cross-sectional Data. Ann Intern Med. 2014; 161(7):482-490. http://annals.org/article.aspx?articleid=1911118
6) Cudkowicz ME, Titus S, Kearney M, et al. Safety and efficacy of ceftriaxone for amyotrophic lateral sclerosis: a multi-stage, randomised, double-blind, placebo-controlled trial. Lancet Neurol. Published online 10/6/2014. http://www.thelancet.com/journals/laneur/article/PIIS1474-4422%2814%2970222-4/abstract.
7) Kalil AC, Van Schooneveld TC, Fey PD, et al. Association between vancomycin minimum inhibitory concentration and mortality among patients with Staphylococcus aureus bloodstream infections. JAMA. 2014; 312(15):1552-1564. http://jama.jamanetwork.com/article.aspx?articleid=1913620
8 ) Stacy SR, Suarez-Cuervo C, Berger Z, et al. Role of troponin in patients with chronic kidney disease and suspected acute coronary syndrome: a systematic review. Ann Intern Med. 2014; 161(7):502-512. http://annals.org/article.aspx?articleid=1895