Peer Reviewed
Last week, the nation focused on the Northeast, as it was battered by winter storm Jonas. This week, the nation again turns its collective attention eastward. The Iowa caucuses start Monday, and with them the race to the White House begins in earnest. Clinton continues to hold the lead over Sanders and O’Malley, while Cruz and Trump are battling for a last minute advantage [1]. The less politically inclined have another contest to look forward to. This one in Santa Clara, where the Carolina Panthers will be battling the Denver Broncos. Meanwhile, the Zika virus continues to dominate the medical news as it sweeps across the Americas, with over 20,000 confirmed cases in Colombia alone [2]. Just like the news, this week’s primecuts is a mix of the worrisome, the encouraging, the controversial and the important.
New Highly Transmissible Polymyxin Resistance Gene Identified in China
Last week, Primecuts reported on a global survey by the WHO which showed widespread misunderstanding of antibiotic resistance [3]. Now, we report on more discouraging news in the fight against antibiotic resistance.
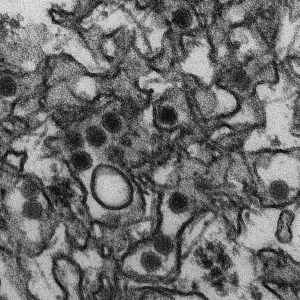
This week, researchers announced that they have found the gene for polymyxin resistance in plasmids in pig farms [4]. Pig farms are among the biggest users of polymyxin, and use a large share of the approximately 12,000 metric tons used annually in agricultural uses [5]. The gene, dubbed plasmid-mediated colistin resistance 1 (mcr-1) was found in strains of E. coli collected from outside of Shanghai, China. Most concerning is that researchers were able to demonstrate the easy transmissibility of mcr-1 into other strains of E. coli as well as Klebsiella and Pseudomonas. Previous reports of polymyxin resistance have been limited to chromosomal mutations, which are not easily transferred between organisms [6].
Subsequent screening for the mcr-1 gene revealed that more than 20% of pigs screened carry bacteria that harbor this gene. This same gene was also identified in isolates from human inpatients with Klebsiella and E. coli infections. The presence of a highly transmissible gene for polymyxin resistance, now identified in pigs and humans in China, raises the specter of a future of pan-resistant infections. Urgent action is needed to limit the agricultural use of polymyxin, and to develop new antibiotics to prevent the spread of treatment-resistant infections.
New Osteoarthritis Intervention Shows Statistical, but not Clinical Improvement in Pain and Function
Evidence based management of osteoarthritis (OA) requires both behavior changes (e.g. weight loss, exercise) and clinical interventions (e.g. physical therapy, joint injections, joint replacement) [7]. Considering the high prevalence of OA, and detrimental effect on a patient’s quality of life, many of these interventions are unfortunately underutilized. To address this issue, researchers at the VA Medical Center in Durham, North Carolina piloted a novel intervention targeting both providers and patients [8].
Primary care providers (PCPs) were randomized into two groups. Fifteen PCPs in the intervention group received patient-specific recommendations for OA treatment via their electronic medical record system. Recommendations based on a review of the patient’s record included referral to a physical therapist, weight loss program or orthopedic surgeon, and specific recommendations for medications and joint injections. The remaining fifteen PCPs had no intervention and continued with usual care of their patients. The study enrolled 300 patients, evenly split between intervention and usual care providers. Patients of PCPs in the intervention arm received one year of telephone calls with a counselor who employed motivational interviewing techniques focused on weight management and increasing physical activity. The control group received usual care.
The primary outcome was the score on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) which measures pain, stiffness, and function. At 12 months, the intervention group showed an improvement of approximately 9% in WOMAC scores. This falls short of the threshold for clinically significant improvement of 12-18% [9]. Although the study failed to show clinical significance in its primary endpoint, there was a clinically significant increase of 3.6 hours in physical activity per week in the intervention group. The modest improvement in WOMAC scores following this intervention suggests higher intensity interventions are needed to gain clinically meaningful improvements in pain and function.
No Mortality Benefit with Corticosteroids in Community-Acquired Pneumonia
There has been an increased interest in the role of corticosteroids in the treatment of community-acquired pneumonia (CAP) since a report in JAMA last year showed decreased treatment failure with the addition of corticosteroids [10]. A new meta-analysis published in Chest this week, synthesizes the available data on corticosteroids in CAP [11].
Across 1700 patients in nine randomized controlled trials (including the JAMA article mentioned above), researchers found no overall difference in mortality (RR, 0.72; 95% CI, 0.43-1.21). Among the five trials that reported mortality in patients with severe CAP, there was also no difference in mortality (RR, 0.64; 95% CI, 0.32-1.29). Heterogeneity among the studies was low (I2 =27% and 0% respectively). Corticosteroids were not associated with adverse events, including gastrointestinal bleeding, super-infection, and hyperglycemia. Across all patients there was a decreased risk of acute respiratory distress syndrome (ARDS) (RR, 0.21; 95% CI, 0.08-0.59). These results must be interpreted with caution. The quality of the articles was low with a high risk of bias, as assessed using the GRADE criteria, a standardized system for evaluating articles in meta-analyses [12]. It does, however, suggest a possible role for steroids in the prevention of ARDS in selected patients. More research is needed before any firm recommendations can be made.
New Strategies for Decreasing Antibiotic Use in Upper Respiratory Infections
Despite the fact that most upper respiratory infections are viral in origin and self limited in nature, many patients who visit their doctors still leave with a prescription for antibiotics [13]. A new study in JAMA Internal Medicine examines strategies for reducing antibiotic use in these patients [14]. Four hundred participants were randomized to one of four strategies: (1) immediate prescription for antibiotics, (2) no prescription, (3) a prescription that participants could collect at their PCP’s front desk after three days, or (4) a prescription which participants were told to fill after three days. There was a substantial decrease in the number of antibiotic prescriptions that were filled, from 91% in the immediate antibiotics group to 12% in the no prescription group (P <0.01). Having patients collect their prescription from their PCP after three days, or instructing patients to fill the prescription only after three days also substantially decreased antibiotic usage compared to immediate prescription (23% and 32% respectively, P <0.01). Patient satisfaction was similar across all groups and there was no difference in complications, adverse events, or need for unscheduled care among the four groups.
There was an increase in duration of severe symptoms, from 3.6 days in the immediate prescription group, to 4.7 days in the no prescription group. There were similar increases in duration of symptoms of moderate intensity, and for three out of five individual symptoms. These data should be interpreted with caution. The article does not address allocation concealment, and there were significantly more participants in the no prescription group who believed that antibiotics are ineffective (8% in the prescription group, versus 20% in the no prescription group). The strategies outlined in this article could be helpful in reducing unnecessary antibiotic use in the primary care setting and preventing the spread of antibiotic resistance without compromising patient safety or satisfaction. However, further research is needed to understand if antibiotics can really impact the duration of upper respiratory tract infections or is this just a powerful placebo effect.
Mini Cuts
Also in the journals this week…
A meta-analysis of the safety and efficacy of the once weekly GLP-1 receptor agonists showed the greatest reduction in A1c and body weight with duraglutide, exenatide and taspoglutide [15]. There was little difference in risk of hypoglycemia, though taspoglutide was associated with a greater risk of nausea.
The authors of the BENEFIT trial reported their final results this week after seven years of follow-up in recipients of kidney transplants. Compared to cyclosporine, belatacept was associated with significantly better GFR and graft survival [16]. This could herald a major shift in the treatment of renal transplants.
The ROCKET AF trial compared warfarin to rivaroxaban in the treatment of atrial fibrillation. A new analysis of the data from this trial shows a decreased risk of bleeding when rivaroxaban is used compared to warfarin in patients taking 0-4 concomitant medications. This potential benefit is lost when patients are on 5 or greater medications. [17].
Dr. Kevin Hauck is an Instructor of Medicine, Tisch Hospital Inpatient Site Director, NYU Internal Medicine Residency Program, NYU Langone Medical Center
Reviewed by Neil Shapiro, MD, Editor-In-Chief, Clinical Correlations
Image courtesy of Wikimedia Commons
References
[1] Boyce, J, et al., 2016 Primary Forecasts. FiveThirtyEight. Published January 30, 2016. http://projects.fivethirtyeight.com/election-2016/primary-forecast/iowa-republican/
[2] Reuters. Colombia Reports More Than 2,100 Pregnant Women Have Zika Virus. The New York Times. Published January 30, 2016. http://www.nytimes.com/2016/01/31/world/americas/colombia-reports-more-than-2100-pregnant-women-have-zika-virus.html?ref=health&_r=0
[3] WHO. Antibiotic resistance: multi-country awareness survey. World Health Organization. 2015. http://apps.who.int/iris/bitstream/10665/194460/1/9789241509817_eng.pdf
[4] Liu, YY, et al., Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. The Lancet Infectious Diseases. 2016; Volume 16 , Issue 2 , 161-168. Available online at: http://www.thelancet.com/journals/laninf/article/PIIS1473-3099(15)00424-7/abstract
[5] QYResearch Medical Research Center. The global polymyxin industry report 2015. 2015; August. http://www.qyresearch.com
[6] Kempf, I, et al., What do we know about resistance to colistin in Enterobacteriaceae in avian and pig production in Europe? Int J Antimicrobial Agents. 2014; Volume 42, 379-83.
[7]Hochberg, MC, et al., American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012; Volume 64, Issue 4, 465-474.
[8] Allen, KD, et al., A Combined Patient and Provider Intervention for Management of Osteoarthritis in Veterans. Annals of Internal Medicine. Volume 164, Issue 2, 73-83. Available online: http://annals.org/article.aspx?articleid=2478159
[9] Ehrich, E, et al., Minimal perceptible clinical improvement with the Western Ontario and McMaster Universities Osteoarthritis Index questionnaire and global assessments in patients with osteoarthritis. J Rheumatology. 2000; Volume 27, 2635-2641.
[10] Torres A, et al., Effect of Corticosteroids on Treatment Failure Among Hospitalized Patients With Severe Community-Acquired Pneumonia and High Inflammatory Response: A Randomized Clinical Trial. JAMA. 2015; Volume 313, Issue 7, 677-686. Available online at: http://jama.jamanetwork.com/article.aspx?articleid=2110967
[11] Wan, Y, et al., Efficacy and Safety of Corticosteroids for Community-Acquired Pneumonia: A Systematic Review and Meta-Analysis. Chest. 2016; Volume 149, Issue 1, 209-219. Available online at: http://journal.publications.chestnet.org/article.aspx?articleid=2466639
[12] Higgins, J, Green, S, Cochrane handbook for systematic reviews of interventions, version 5.1.0 [updated march 2011]. Cochrane Collaboration. Available at: http://handbook.cochrane.org/
[13] Barnett ML, Linder JA. Antibiotic prescribing for adults with acute bronchitis in the United States, 1996-2010. JAMA. 2014; Volume 311, Issue 19, 2020-2022.
[14] de la Poza, A, et al., Prescription Strategies in Acute Uncomplicated Respiratory Infections: A Randomized Clinical Trial. JAMA Intern Med. 2016; Volume 176, Issue 1, 21-29. Available online at: http://archinte.jamanetwork.com/article.aspx?articleid=2475025
[15] Zaccardi F, et al., Benefits and Harms of Once-Weekly Glucagon-like Peptide-1 Receptor Agonist Treatments: A Systematic Review and Network Meta-analysis. Ann Intern Med. 2016 Volume 164, Issue 2, 102-113. Available online at: http://annals.org/article.aspx?articleid=2474362
[16] Vincenti, F., et al., Belatacept and Long-Term Outcomes in Kidney Transplantation. NEJM. 2016; Volume 374, Issue 4, 333-343. Available online at: http://www.nejm.org/doi/full/10.1056/NEJMoa1506027
[17] Piccini, J, et al., Polypharmacy and the Efficacy and Safety of Rivaroxaban versus Warfarin in the Prevention of Stroke in Patients With Nonvalvular Atrial Fibrillation. Circulation. 2016; Volume 133, 352-360. Available online at: http://circ.ahajournals.org/content/early/2015/12/16/CIRCULATIONAHA.115.018544.abstract