Peer Reviewed
This past week marks the first leg of president Trump’s foreign trip starting at Saudi Arabia, where he was lavished with extravagant gifts. While former president Obama slowed military cooperation with the kingdom from the concerns of the country’s indiscriminate bombing of civilians in Yemen, Trump may seek to expand them.
The number of suspected cases of Ebola has now risen to 29 in less than a week the Democratic Republic of Congo. The risk of spread is high given the level of surveillance and access to healthcare. Aid groups are struggling to reach the area given road conditions.
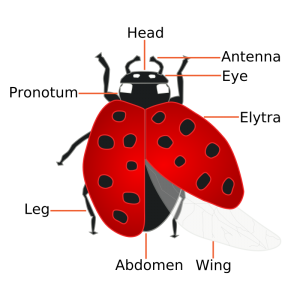
In other news, Dr. Saito from the University of Tokyo have engineered an artificial wing in the ladybug in order to study rapid, repetitive storage and deployment of parachute like objects, learning a valuable lesson for engineering deployable structures such as umbrellas and satellites.Â
PrimeCuts Â
Novel Noninvasive Measurement of Inflammation in Crohn’s Patients [1]
Multispectral optoacoustic tomography (MSOT) is an imaging technique that emits short pulsed laser light with near infrared wavelength (700 – 900 nm) towards target erythrocytes in the small and large bowel. Through thermoelastic expansion of the erythrocytes, detectable soundwaves return as measurements of total, oxygenated, and deoxygenated hemoglobin. The quantification of tissue oxygenation and perfusion allows for surrogate measurement of the extent of inflammation in the bowel.
In this single-center, cross-sectional study published in NEJM, 107 patients with various degree of Crohn’s disease activity were evaluated using MSOT. Patients with active and non-active diseases were determined clinically (Harvey-Bradshaw index), endoscopically (simplified endoscopic score for Crohn’s disease, or SES-CD), and histologically (modified Riley score). MSOT were also referenced against conventional ultrasound techniques, which measures intestinal wall thickness and perfusion (Limberg score). Six different wavelengths were tested, yielding levels total, oxygenated, deoxygenated hemoglobin as well as oxygen saturation as measurements of Crohn’s activity.
Using endoscopy (n = 44) and histology (n=42) as reference values, there were significant (P<0.001) differences in MSOT values comparing patients with active versus non-active disease, especially at wavelengths of 760nm. Significant differences were also found between patients in remission and those with low grade active disease (P=0.02, P0.03 respectively). However, with only clinical scoring (n=86) as the only reference point, MSOT was unable to yield clinically significant measurements, suggesting that at present MSOT along may not replace invasive diagnostics entirely.
The study was limited by small sample size and lack of external validation. MSOT technology may also be operator dependent given that 17 patients were excluded because they could not be evaluated. Given the risks and preprocedural prep required of invasive imaging in Crohn’s patient to detect disease activity with treatment, MSOT provides a new alternative towards noninvasive options for distinguishing active disease from remission in patients with Crohn’s disease.
Teprotumumab Targeting Thyroid- Associated Opthalmopathy [2]
Current treatments of Graves showed marginal effects on proptosis. High dose glucocorticoids and radiotherapy have mostly shown benefit in reducing symptoms of inflammation. The rational for treatment ineffectiveness may stem from incompletely understanding the pathophysiology of Graves opthalmopathy, the mechanism which is mediated by autoantibody stimulation of the thyrotropin receptor. Thyrotropin receptors, however, are not always detected in orbital tissues, suggesting that additional autoantibodies may be involved in the disease process.
IGF-1 and its receptor IGF-1R have been shown to be overexpressed by orbital fibroblasts, T cell, and B cells in Graves disease. Activation of IGF, IGF-1R may synergistically enhance the action of thyrotropin. Inhibitory antibodies targeting IGF-1R can therefore attenuate the actions of IGF-1, thyrotropin, and thyroid stimulating immunoglobulins. Teprotumumab is such a monoclonal antibody inhibiting IGF-1R.
In this article, Smith et al conducted a multi-center, double blinded, randomized, controlled trial comparing teprotumumab versus placebo in patients with active moderate to severe opthalmopathy. Patients were diagnosed 9 months after onset of symptoms, have not received surgical or medical treatment other than oral glucocorticoids. Patients were assessed every 3 weeks until total of 48 weeks.
Response was measured using a 7 point score for clinical activity, exopthalmometer for proptosis, and questionnaire for quality of life.
Eighty-eight patients were randomized. Scores were identical at onset, and at week 24 Teprotumumab was shown to be statistically more effective than placebo in reducing both proptosis and clinical activity score (Intention to treat AOR 8.86, P<0.001, per protocol AOR 12.73, P<0.001). The treatment group also showed statistically more rapid onset, faster time to first response, further reduction in activity score, sustained improvement throughout the treatment course, as well as improved quality of life scores.
Teprotumumab was associated with hyperglycemia, worse in patient with preexisting diabetes, requiring some titration of diabetic medication to achieve optimum control. The safety profile of the medication was encouraging. The trial is limited by enrolling patients only with active disease of recent onset and those with severe clinical activity score. Thus the benefit of treatment on milder cases are still unclear, and longer term follow up beyond 24weeks may be necessary.
Bystander Efforts and 1-Year Outcomes in Out-of Hospital Cardiac Arrest [3]
The rates of hospital survival after out of hospital cardiac arrest due to improvement in public awareness and in post-CPR care in the hospital. However, little is known about subsequent long term outcomes, specifically post cardiac arrest such as anoxic brain injury, limited activities of daily living, and nursing home admissions. Using the Denmark EMS Cardiac Arrest Registry, Kragholm et al included all people 18 years and older who were 30 day survivors of out-of-hospital cardiac arrest from 2001 to 2012. Follow up data was obtained from national registries and national nursing home admission data.
Between 2001 to 2012, 2855 (8.3%) patients who had an out-of-hospital cardiac arrest, whom resuscitation was attempted, and who survived for 30 days were included in the study. In comparison to prior data, the percentage of 30-day survival over 10 years has increased from 3.9% to 12.4%. From initial demographics of the 30-day survivor group showed that the bystander CPR, defibrillation group had greater proportions of men, witnessed arrest, public location of arrest and lower Charleston comorbidity index scores.
Upon 1 year follow up, 276 (9.7%) out of the 2855 patients died, of which 197 (71.4) had a presumed cardiovascular cause. Three hundred (10.5%) had anoxic brain damage or were admitted to the nursing home of which 59 died within 1 year. The median time between event or nursing home admission to death was 85 days. Between 2001 to 2012 the rates of bystander intervention increased while the proportion of negative outcomes decreased. Compared to no intervention, initial intervention with bystander CPR or defibrillation was associated with lowered risk of all cause mortality, anoxic brain damage, or nursing home admission.
The lowest absolute risk was seen in EMS-witness cardiac arrest (3.7% 95% CI 2.5 – 4.9), lowest risk of death seen in bystander-defibrillation group (2%, 95% CI 0 – 4.2). The highest risk of anoxic brain injury and nursing home admission was seen in the no bystander resuscitation group (18.6%, 95% CI 16 -22.2). All cause mortality was also higher in the no bystander resuscitation group (15.5% 95% CI 12.5-18.6). The results suggest that bystander out of hospital resuscitation of cardiac arrest was associated with lower 1 year risk of morbidity and mortality. Over the course of the study over 10 years, with increasing rates of bystander out of hospital resuscitation was associated with lower rates of morbidity and mortality.
KIT Inhibition by Imatinib in Patients with Severe Refractory Asthma [4]
Targeted therapy towards treatment of airway hyperresponsiveness may lead to more effective symptom control in asthma. Difficult to control asthma has been shown to have high levels of tryptase, surrogate for mast cell burden and degranulation, in bronchoalveolar washings. Despite glucocorticoid treatments, mast cells may continue to survive due to presence of long living hematopoietic effector cells. Imatinib inhibits tyrosine kinase activity of receptor KIT protooncogene, which is a stem cell factor essential for mast cell survival. Currently imatinib is used for treatment of patients with chronic myeloid leukemia and pulmonary hypertension but this mechanism may extend to treating patients with refractory asthma.
This was a randomized, double blind, placebo, proof of principal trial involving 7 academic centers from 2010 to 2015. The study enrolled patients ages 18-65, with severe refractory asthma not controlled despite inhaled beclamethasone, with Asthma Control Questionnaire (ACQ-6) score 1.5 or higher, FEV1 decrease of over 20% upon methacholine challenge, and a FEV1 at 40% of predicted value. Patients were randomized to imatinib 200mg per day for 2 weeks then 400mg per day versus placebo. Both medications were dosed once daily.
Bronchoscopy and airway biopsy were performed before randomization and repeated at week 24. The primary outcome measured were change in airway hyperresponsiveness as PC20 score (concentration of methacholine needed to produce a 20% fall in FEV1 from baseline). Secondary outcomes measured were FEV1, peak expiration flow, mast cell count, tryptase level, and smooth muscle biopsy samples. In addition, blood eosinophil, histamine, leukotriene, and prostaglandins were measured. Also assessed were allergy skin testing, asthma symptom index, and patient reported quality of life questionnaire.
One hundred seventy-six patients were screened and 62 were equally randomized, no significant differences were noted in baseline characteristics. For primary outcome, imatinib was noted to increase methacholine PC20 by mean of 1.2 + 0.52 doubling doses from baseline by month 3 (P = 0.03), 1.73 + 0.6 by month 6 (P = 0.008) compared to 0.03 +0.42 (P = 0.94) and 1.07 + 0.6 (P= 0.08) respectively of the placebo group. Difference between treatment and placebo over course of trial was P = 0.048.
Regarding secondary outcomes, total and BAL tryptase level decreased in imatinib and increased with placebo. Mast cell count both decreased without statistically significance towards greater reduction in the treatment group. Treatment group had fewer asthma exacerbations, greater reduction airway wall thickness, higher peak expiratory flows, and greater improved patient reported outcomes however were not statistically significant. No significant differences were found for counts of eosinophil, histamine, leukotriene, prostaglandins. Side effects did not differ significantly between groups and included muscle cramps and metabolic abnormalities which abated since discontinuing treatment.
In conclusion, imatinib was associated with clinically significant increase in FEV1 and improvement in PC20 scores that correlated with reductions in endobronchial mast cell counts which may help support the role of mast cells in persistent refractory asthma. The improvements may be secondary to imatinib’s inhibition of lymphoid cell producing cytokines causing eosinophilic and neutrophilic inflammation, as well as platelet derived growth factors. Mast cells also were not completely eliminated at 6 months of treatment. This study should be expanded upon with larger and longer trials.Â
MiniCuts Â
New Development on Zika Virus Vaccines [5]
The Zika virus epidemic which started in 2015 brings about intersection of global public health and the debate on elective termination of pregnancy. Currently there are no licensed vaccine or antiviral drug to prevent or treat Zika. Recent reports described successful testing of experimental Zika vaccine in animal models involving engineered mRNAs encoding the viral precursor membrane glycoprotein and envelope glycoprotein critical to viral attachment and replication. Vaccinated mice showed development of binding IgG antibodies and neutralizing antibodies as well as antigen specific CD4+ T cells after vaccination. The same mice were protected from viremia when later challenged with a strain of the Zika.Â
Compound Accumulation Rules in Designing The Next Broad-Spectrum Antibiotic. [6]
Since the quinolones, no new class of antibiotics have been introduced that targets gram negative bacteria. The ideal small molecule must traverse porins through the membrane bilayer faster than they are pumped out through efflux pumps. This article assembles a complex, structurally diverse set of 100 compounds and tested them on E coli, then using computer analysis to yield predictive guidelines for small molecule accumulation in Gram negative bacteria. Testing compounds showed benefit of an ionizable nitrogen embedded in a compound with strict geometric constraints, with diminished accumulation with increasing substitution on the amine group.
New articles published in Science Translational Medicine described combining immune checkpoint blockade with angiogenesis inhibition to improve targeted elimination of cancer cells. Angiogenesis inhibitors promotes vascular normalization and limit the development of dysfunctional tumor vessels. Antibody target angiopoetin (ANG2) and vascular endothelial growth factor (VEGFA) in mouse models of breast, pancreatic, colon cancer and melanoma were shown to promote lymphocyte infiltration and activity.
Dr. Michelle Lo is a resident at NYU Langone Medical Center
Peer reviewed by David Kudlowitz, MD, department of medicine, NYU Langone Medical Center
Image courtesy of Wikimedia Commons
ReferencesÂ
[1] Knieling, F et al. Multispectral Optoacoustic Tomography for Assessment of Crohn’s Disease Activity. N Engl J Med. 2017 Mar 30.  Accessed May 20. http://www.nejm.org.ezproxy.med.nyu.edu/doi/full/10.1056/NEJMc1612455
[2] Smith, T. J. et al. Teprotumumab for Thyroid-Associated Opthalmopathy. N Engl J Med. 2017 May 4. Accessed May 20. http://www.nejm.org.ezproxy.med.nyu.edu/doi/full/10.1056/NEJMoa1614949
[3] Kragholm, K et al. Bystander Efforts and 1-Year Outcomes in Out-of Hospital Cardiac Arrest. N Engl J Med. 2017 May 4. Accessed May 21. http://www.nejm.org.ezproxy.med.nyu.edu/doi/pdf/10.1056/NEJMoa1601891
[4] Cahill, K N. et al. KIT Inhibition by Imatinib in Patients with Severe Refractory Asthma. N Engl J Med. 2017 May 18. Accessed May 21. http://www.nejm.org.ezproxy.med.nyu.edu/doi/pdf/10.1056/NEJMoa1613125
[5] Thomas, S J. Zika Virus Vaccines – A Full Field and Looking for the Closers. N Engl J Med. 2017 May 11. Accessed May 20. http://www.nejm.org.ezproxy.med.nyu.edu/doi/full/10.1056/NEJMcibr1701402
[6] Richter, M. F. et al. Predictive compound accumulation rules yield a broad-spectrum antibiotic. Nature. 2017 May 18. Accessed May 20. http://www.nature.com.ezproxy.med.nyu.edu/nature/journal/v545/n7654/pdf/nature22308.pdf
[7] Villanueva M. T. et al. T cells get a ride. Nature Reviews Drug Discovery. Nature. 2017 May 19. Accessed May 20. http://www.nature.com.ezproxy.med.nyu.edu/nrd/journal/vaop/ncurrent/pdf/nrd.2017.103.pdf