 Commentary by William Slater, MD Associate Professor of Medicine, Divsion of Cardiology
Commentary by William Slater, MD Associate Professor of Medicine, Divsion of Cardiology
The vast majority of patients with persistent AF can be rendered asymptomatic with AV nodal blocking drugs and don’t require ablation. Digitalis is underused but is often of major benefit, either
alone, or in combination with beta blockers or calcium channel blockers.
Of paroxysmal fibrillators, most can be managed by reassurance that the episodes are harmless with a normal heart and of minimal risk if brief even in context of heart disease. The inappropriate fear of stroke drives many patients to seek a definitive “cure”. “Pill in the pocket” therapy, either with Propranolol and Xanax is usually effective; if not, a “cocktail” dose of an antiarrhythmic (Flecainide, Propafenone, or Disopyramide) will often terminate occasional PAF episodes and make ablation unnecessary. Remember that upwards of 20% of ablations for AF result in the creation of a new arrhythmia (an intra-atrial tachycardia) requiring a second procedure, which is not always curative. Ablation is still an evolving technique, and is not appropriate for the majority of atrial fibrillators.
The AFFIRM and RACE studies confirmed that by an “intention to treat” analysis, older patients in AF are just as well treated with a rate control strategy. However, of those treated with rhythm control who actually maintained NSR, they lived longer and had a better quality of life. So, it’s not as simple as treating everyone with rate control. Most younger patients probably benefit from maintenance of NSR. This can be achieved through “cocktail therapy”, antiarrhythmics, or ablation.
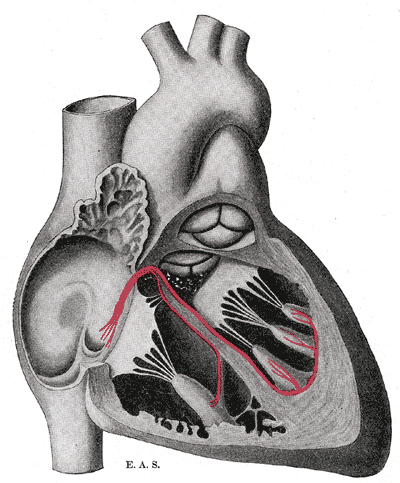
Image courtesy of Gray’s anatomy
