 Commentary by Matt LaBarbera MD, PGY-3 and Rob Donnino, MD Instructor of Medicine, Division of Cardiology
Commentary by Matt LaBarbera MD, PGY-3 and Rob Donnino, MD Instructor of Medicine, Division of Cardiology
Coronary CT angiography (CCTA) is a noninvasive imaging modality which can be used to evaluate the anatomy of the coronary arteries. Unlike coronary artery calcium scoring, which utilizes noncontrast CT to assess atherosclerotic disease burden, CCTA allows direct visualization of the coronary artery wall and lumen with the administration of intravenous contrast. The degree of coronary luminal stenosis can be reliably estimated, as can the presence or absence of both calcified and non-calcified plaques. When compared to invasive quantitative coronary angiography, newer-generation CT scanners have been found to have sensitivities and specificities of over 90%, and negative predictive values of up to 100% for the exclusion of obstructive coronary artery disease (CAD) for both native arteries as well as bypass grafts.[1-5] With recent advances in CT technology and increased availability, CCTA has become a non-invasive alternative for imaging the coronary arteries in an increasing number of patients, and may obviate the need for coronary artery catheterization in some patients.
CCTA can be an effective diagnostic tool for select patients presenting to the emergency room with acute chest pain. With its high negative predictive value, a normal CCTA scan can effectively rule out obstructive CAD in low- and intermediate-risk patients (i.e. those with negative cardiac enzymes and no ECG changes) . [6,7] Some studies have shown that the use of CCTA may decrease hospital admission time as well as improve cost effectiveness compared to traditional diagnostic strategies used to evaluate acute chest pain.[8] The American College of Cardiology (ACC) appropriateness guidelines support the use of CCTA in intermediate-risk patients presenting with acute chest pain. [9]
CCTA may also be helpful in low- and intermediate-risk patients with subacute or chronic chest pain syndromes. While traditional non-invasive testing for CAD is most often done by stress testing (with or without imaging), CCTA may provide additional important clinical information. One of the more common uses of CCTA in current clinical practice is to evaluate for CAD in patients with “equivocal” or “nondiagnostic” stress tests. Alternatively, CCTA can be used in place of stress testing as the initial test to evaluate for CAD. Since CCTA does not provide any functional information, however, it is usually recommended as the initial test only for those who have an uninterpretable baseline ECG or are unable to exercise. [9] The use of CCTA in high risk patients with chest pain is generally not recommended, as these patients often require cardiac catheterization.
The use of CCTA as a screening test for detecting coronary artery disease in asymptomatic patients with traditional risk factors is controversial, and has not been widely recommended. [9] Coronary imaging using CCTA does have some advantages over traditional imaging techniques in its ability to detect small amounts of non-obstructive plaque in the wall of the arterial lumen that might not be detected by stress testing or even invasive angiography. The ability of CCTA to detect these non-obstructive plaques has been validated in studies comparing CCTA with coronary intravascular ultrasound.[2] The optimal strategy for management of asymptomatic CAD found on CCTA, however, has not been determined. Currently, the detection of CAD (both obstructive and non-obstructive) by CCTA in asymptomatic patients raises several questions: Does the presence of mild non-obstructive CAD in an otherwise healthy individual warrant immediate and life-long treatment with a statin? Will treatment with a statin alter the natural progression of coronary disease found on screening CCTA? Does the finding of “clean” coronaries on CCTA in a patient with traditional risk factors reduce the urgency for aggressive lifestyle modification and medication therapy? Further studies are needed to provide guidance with regards to these matters. The radiographic finding of coronary artery disease may have a psychological impact on the patient that may facilitate lifestyle modification and medication compliance; there is evidence, however, that screening for atherosclerosis with coronary calcium scoring has no effect on modification of cardiac risk profile at one year, and it may be argued that patients with traditional risk factors ought to undergo aggressive risk factor modification without the need for CCTA.[10,11]
The use of CCTA is not without risks. CCTA involves a significant radiation exposure, on the order of 10 – 20 mSv (chest x-ray is about 0.05 mSv; technetium stress test is about 10 – 12 mSv; thallium stress test is about 25 – 30 mSv). New, widely-available “dose modulation” techniques, however, can lower average radiation exposure of CCTA to approximately 7-9 mSv. Experimentally, scans have been obtained with as little as 1-2 mSv.[12] As with any test using intravenous contrast, contrast-induced nephropathy may also occur, although the rate of development of end-stage renal disease as a result of contrast administration is very low. [13] Approximately 80-100 ml of contrast are used per study. Anaphylactic reactions to contrast are rare but potentially fatal events. Furthermore, there is concern over incidental findings that may be seen tissues surrounding the heart, such as nodules in the lung or liver which would then need to be addressed clinically. Finally, CCTA currently costs approximately $1,000-$1,500 per scan. The widespread use of CCTA in addition to other imaging modalities would place an obvious financial burden on the health care system. While some advocate that CCTA might reduce overall cost by reducing unnecessary cardiac catheterizations and/or stress tests, more data on cost analysis would be necessary to draw this conclusion. Further studies are warranted assessing the risks and benefits of CCTA to detect CAD in select populations, and patients should be carefully selected to undergo CCTA.
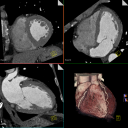 CCTA is a rapidly evolving technology, and newer-generation CT scanners have improved spatial and temporal resolution that makes CCTA a reliable method to identify coronary atherosclerosis. Given its very high negative predictive value, CCTA can reliably exclude obstructive CAD in low- and intermediate-risk patients with both acute and chronic chest pain syndromes, and may obviate the need for coronary catheterization in some patients. Further studies are needed to assess the potential role if any for CCTA in screening asymptomatic patients who are at risk for CAD. Radiation exposure, contrast administration, cost, and the management of incidental findings are all concerns regarding CCTA. While new advances in this rapidly evolving technology will likely improve the safety and accuracy of CCTA, these risks must be weighed against the potential benefits.
CCTA is a rapidly evolving technology, and newer-generation CT scanners have improved spatial and temporal resolution that makes CCTA a reliable method to identify coronary atherosclerosis. Given its very high negative predictive value, CCTA can reliably exclude obstructive CAD in low- and intermediate-risk patients with both acute and chronic chest pain syndromes, and may obviate the need for coronary catheterization in some patients. Further studies are needed to assess the potential role if any for CCTA in screening asymptomatic patients who are at risk for CAD. Radiation exposure, contrast administration, cost, and the management of incidental findings are all concerns regarding CCTA. While new advances in this rapidly evolving technology will likely improve the safety and accuracy of CCTA, these risks must be weighed against the potential benefits.
References:
1. Meijboom et al. 64-Slice Computed Tomography Coronary Angiography in Patients With High, Intermediate, or Low Pretest Probability of Significant Coronary Artery Disease. Journal of the American College of Cardiology. 50(15); 1469-1475, Oct 2007.
2. Leber et al. Quantification of Obstructive and Nonobstructive Coronary Lesions by 64-Slice Computed Tomography: A Comparative Study With Quantitative Coronary Angiography and Intravascular Ultrasound. Journal of the American College of Cardiology. 46(1); 147-154, July 2005.
3. Mollet et al. High-Resolution Spiral Computed Tomography Coronary Angiography in Patients Referred for Diagnostic Conventional Coronary Angiography. Circulation. 112(15); 2318-2323, Oct 2005.
4. Jones et al. Multi-Detector Computed Tomography in Coronary Artery Bypass Graft Assessment: A Meta-Analysis. Annals of Thoracic Surgery. 83(1);341-348, Jan 2007.
5. Hamon et al. Diagnostic Performance of Multislice Spiral Computed Tomography of Coronary Arteries as Compared With Conventional Invasive Coronary Angiography: A Meta-Analysis. Journal of the American College of Cardiology. 48(9); 1896-910, Nov 2006.
6. Gallagher et al. The Diagnostic Accuracy of 64-Slice Computed Tomography Coronary Angiography Compared With Stress Nuclear Imaging in Emergency Department Low-Risk Chest Pain Patients. Annals of Emergency Medicine. 49(2); 125-136, Feb 2007.
7. Goldstein JA et al. A Randomized Controlled Trial of Multi-Slice Coronary Computed Tomography for Evaluation of Acute Chest Pain. Journal of the American College of Cardiology. 49(8); 863-71, Feb 2007.
8. Powell et al. Cost Analysis of CT Coronary Angiography in Observation Unit Patients after Positive or Indeterminate Stress Tests. Annals of Emergency Medicine. 50(3); S48, September 2007.
9. Hendel et al. ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 Appropriateness Criteria for Cardiac Computed Tomography and Cardiac Magnetic Resonance Imaging: A Report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. Journal of the American College of Cardiology. 48(7); 1475-1497, Oct 2006.
10. O’Malley PG et al. Impact of Electron Beam Tomography, With or Without Case Management, on Motivation, Behavioral Change, and Cardiovascular Risk Profile: A Randomized Controlled Trial. Journal of the American Medical Association. 289(17); 2215-2223, May 7 2003.
11. Kalia et al. Visualizing coronary calcium is associated with improvements in adherence to statin therapy. Atherosclerosis. 185(2); 394-399, April 2006.
12. Husman et al. Feasibility of low-dose coronary CT angiography: first experience with prospective ECG-gating. European Heart Journal. 29(2) 191-197, Jan 2008.
13. Mitchell AM and Kline JA. Contrast nephropathy following computed tomography angiography of the chest for pulmonary embolism in the emergency department. Journal of Thrombosis and Haemostasis. 5(1); 50-54, Jan 2007.
