Vivian Hayashi MD and Robert Smith MD, Mystery Quiz Section Editors
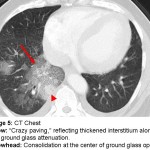
The answer to the mystery quiz is bland alveolar hemorrhage. The CXR (image 1) shows cardiomegaly with mild increase in opacification of the right middle and right lower lobes. The CT images show areas of multifocal ground glass opacification, that is, the underlying interstitium is visible through the opacification, and the variably sized opacities are widely distributed throughout the lungs (images 2, 3, and 4). Image 4 shows prominent interstitium through the ground glass. This pattern is sometimes referred to as “crazy paving” (arrow, image 5). “Crazy paving,” reflecting thickened interstitium along with ground glass attenuation, is often associated with alveolar proteinosis. The radiographic pattern, however, is non-specific and may be seen in any condition in which the interstitium is thickened, as in pulmonary venous congestion, and the alveoli are filled, as in pulmonary hemorrhage. Any alveolar process, such as edema, blood or lipid containing material, may be associated with a ground glass appearance on imaging, as long as the density of the alveolar material does not obscure the underlying lung architecture. Once obscured, the density is considered to be consolidation, as seen in the center of the ground glass opacification (image 5, arrowhead). Image 5 also shows small bilateral effusions.
Alveolar hemorrhage is a syndrome that spans pulmonary vasculitis, including Wegener’s, microscopic polyarteritis, Churg-Strauss, Goodpasture’s, glomerulonephritis with pulmonary hemorrhage, and pulmonary capillaritis. Patients usually present with evidence of systemic inflammation and appear acutely ill. Cases of alveolar hemorrhage may also be associated with drug toxicity that results in diffuse alveolar damage, such as penicillamine or crack cocaine. Other cases may be due to the effects of anticoagulation, possibly exacerbated by increased pulmonary venous pressure as seen in left ventricular failure or valvular disease, such as mitral stenosis. These latter cases are considered to be bland alveolar hemorrhage.
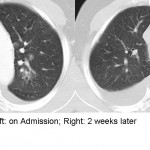
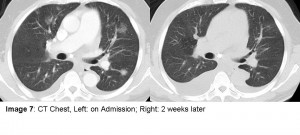
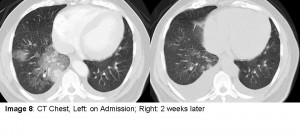
Our patient did not appear acutely ill and the clinical picture did not suggest a vasculitis or infectious disease. Although his INR was only 1.5 on admission, the patient was on enoxaparin and increased pulmonary venous pressures likely contributed to the bland pulmonary hemorrhage. A repeat CT two weeks later (image 6, 7, 8 ) showed resolution of the ground glass opacities and, coincidentally, increased bilateral effusions due to LV failure. An important clinical observation is that bland alveolar hemorrhage will clear quickly, often in just a few days, if the precipitating cause has been eliminated. In contrast, untreated inflammatory disease will usually persist or worsen.