Faculty peer reviewed
At a recent conference on renal transplantation, the importance of early renal biopsy for the diagnosis of acute rejection was emphasized. As busy practitioners of general internal medicine, we rarely have the opportunity to learn the details of a subspecialty procedure such as renal biopsy. However, knowing the details of these procedures is important in providing care for these specific patients. What are the indications, risks, and follow-up care required for the renal biopsy patient? In the native kidney patient, is the renal biopsy an underutilized test?
Renal biopsy is indicated for a myriad of conditions. Renal biopsy should be considered in patients with acute kidney injury after clinical history and physical, lab, and imaging exams fail to diagnose the etiology of the renal insult (1). However, the more specific indications for biopsy are largely a matter of expert opinion. In patients with preserved renal function a commonly accepted indication for biopsy is microhematuria that is associated with greater than 1 g/day of proteinuria. In acute renal failure it is accepted to biopsy when a glomerular lesion is suspected; however experts vary in the appropriate timing of the biopsy. Most experts advocate biopsy immediately or after one week of non-recovery, although some wait up to one month. In chronic kidney disease, most experts would biopsy patients with preserved renal size, except in the USA where small renal size was not a deterrent to biopsy. Almost all experts will biopsy patients with chronic renal insufficiency and nephrotic range proteinuria (2). Also in chronic kidney disease, renal biopsy can confirm the diagnosis by differentiating chronic from acute kidney disease, guide treatment, and provide prognostic information (3). In fact, in a study by Haas et al., renal biopsy results for over one-thousand elderly patients were examined and compared to pre-biopsy clinical diagnoses for the etiology of renal disease. It was found that the pre and post biopsy results only agreed 67% of the time, and that the biopsy provided a diagnosis over 90% of the time (4). This suggests that renal biopsy is an underutilized and important procedure in diagnosing both acute and chronic kidney disease.
Like most invasive procedures in internal medicine, renal biopsy technique has evolved over the years in favor of better patient safety. What used to be a blind manual procedure is now one that is often done under real-time ultrasound guidance and always with a spring-loaded biopsy gun. This has been shown to result in less complications and higher yield of adequate renal tissue for pathologic examination. An interventional radiology transjugular approach is also available in the case of a patient at a very high risk of bleeding (5).
Although the safety of renal biopsy is improving with better technique, the procedure is not without risks. The most common risks are bleeding complications, including hematuria and perinephric or retroperitoneal hematoma. These complications are serious (as defined by requiring blood transfusion, surgical intervention, or other invasive procedures such as angiography and embolization to control bleeding) in less than 1 % or up to 6 % of patients undergoing biopsy, depending on the study. Since almost all of these complications become evident in the first 8-24 hours after biopsy, some authors have recommended that patients should be observed for at least this amount of time before returning home after the procedure. A 24 hour period of observation is more ideal, with measurement of a post-biopsy hematocrit the next day (5, 6). However, in practice, patients are usually observed for about 4-6 hours, and the hematocrit is only checked in cases of suspected bleeding. This allows renal biopsy to be done in the outpatient setting.
The clinical predictors associated with increased risk of bleeding identified in one recent prospective cohort study of 471 patients using modern biopsy technique were female sex, increased baseline PTT, and younger age (7). As with all procedures, the number of passes and the gauge of the biopsy needle are also correlated with the bleeding risk. Some relative contraindications to renal biopsy are uncontrolled hypertension, solitary kidney, hydronephrosis, renal infection, severe anemia, pregnancy, and renal artery aneurysm (5). These factors should be taken into consideration when assessing your individual patient for renal biopsy. Another question that is often raised in the era of drug-eluting coronary stents is the need to stop antiplatelet therapy for a particular procedure. A recently published retrospective study compared patients undergoing elective renal biopsies while on antiplatelet therapy (aspirin and/or clopidigrel) with those that discontinued antiplatelet therapy 5 days prior to biopsy (8). An increase in minor bleeding was seen in the antiplatelet group, but there was no increase in major bleeding, defined as requiring blood transfusion or intervention. Although the event rate was low in the study, and therefore a much larger study would be needed to demonstrate any differences that may exist in the endpoints, it does suggest that renal biopsy while on antiplatelet therapy may be safe in selected patients. This must be weighed against the risk of stopping aspirin and plavix in your individual patient. In practice, renal biopsy on antiplatelet agents is usually reserved for emergent situations, such as acute glomerulonephritis or suspected renal transplant rejection.
Dr. Gandolfo is a 3rd year internal medicine resident at NYU Medical Center.
Faculty peer and commentary below by Alexander Gilbert, M.D. ,Clinical Assistant Professor of Medicine , Division of Neprhology, New York University Medical Center
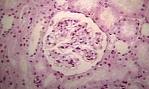
In his review of renal biopsy indications and technique, Dr. Gandolfo discusses the vital role that renal biopsy plays in evaluation of medical renal disease. While the diagnosis of tubular or interstitial disease is often accomplished without need for invasive procedures, the nature of glomerular damage means that while laboratory testing can be helpful and suggestive, renal biopsy remains the “gold-standard” for diagnosing glomerular diseases. As the therapies available for renal disease have diversified, accurate diagnosis of renal disease has become increasingly important. Moreover, the knowledge of specific pathology enables nephrologists to specifically stage and classify the renal disease allowing less toxic or more specific therapies to be used. In addition, with modern processing methods, initial results from a biopsy may be available within 6 hours, faster than most laboratory testing.
In the transplant population, the value of the renal biopsy is even greater. As an example, transplant patients are susceptible to viral nephropathies (treated with a reduction in their immune suppression) and acute rejection (treated with an increase in immune suppression). These conditions, with their diametrically opposed treatments, present identically and are increasingly refractory to treatment when there are delays in diagnosis. As a result, biopsy is often the initial diagnostic test done in the renal transplant patient. Indeed, routine or “protocol” biopsies are being increasingly used in order to make the earliest possible diagnosis of renal pathology.
With the increasing incidence of renal disease, and the rising numbers of kidney transplant recipients, it is of growing importance to be familiar with the risks and benefits of renal biopsy. In his review, Dr. Gandolfo mentions some of the contra-indications to biopsy. It is critical to know when any of these complicating factors are present, but it is also important to realize that none of these are absolute contraindications to biopsy, especially in cases where a rapidly progressive renal disease such as acute rejection or necrotizing crescentic glomerulonephritis are suspected. With new technologies including real-time ultrasound guidance, automatic biopsy needles, and close post-procedure follow-up, renal biopsy can be done as a very safe and effective outpatient procedure for managing renal disease.
1. Saxena R, Toto R. Brenner and Rector’s The Kidney. 8th ed. Philadelphia: Saunders; c2007. Chapter 22, Approach to the patient with kidney disease; p. 710.
2. Fuiano G, Mazza G, Comi N, et al. Current indications for renal biopsy: a questionnaire based survey. Am J Kidney Dis. 2000 Mar;35(3): 448-457.
3. Saxena R, Toto RD. Brenner and Rector’s The Kidney. 8th ed. Philadelphia: Saunders; c2007. Chapter 22, Approach to the patient with kidney disease; p. 713.
4. Haas M, Spargo B, Wit E, et al. Etiologies and outcome of acute renal insufficiency in older adults: a renal biopsy study of 259 cases. Am J Kidney Dis. 2000 Mar 35(3):433-47.
5. Maya I, Allon M, Saddekni S, et al. Brenner and Rector’s The Kidney. 8th ed. Philadelphia: Saunders; c2007. Chapter 28, Interventional nephrology; p. 936.
6. Whittier W, Korbet S. Timing of complications in percutaneous renal biopsy. J Am Soc Nephrol. 2004 Jan;15(1):142-7.
7. Manno C, Strippoli G, Arnesano L, et al. Predictors of bleeding complications in percutaneous ultrasound-guided renal biopsy. Kidney Int. 2004 Oct;66:1570-1577.
8. Mackinnon B, Fraser E, Simpson K, et al. Is it necessary to stop antiplatelet agents before a native renal biopsy? Nephrol Dial Transplant. 2008 Nov;23(11):3566-70.