Vivian Hayashi MD and Robert Smith MD, Mystery Quiz Section Editors
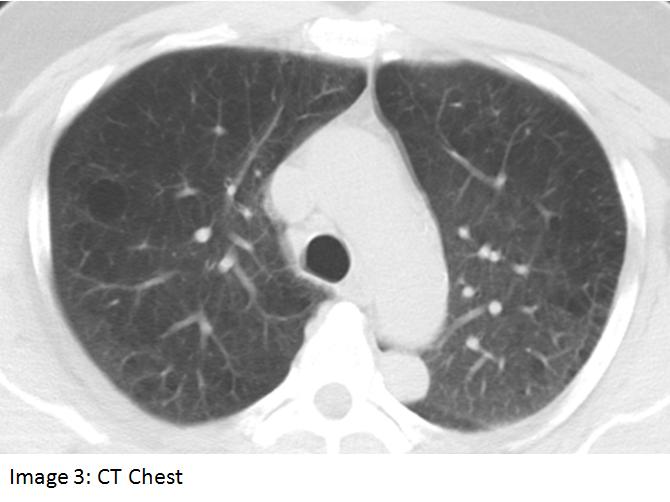
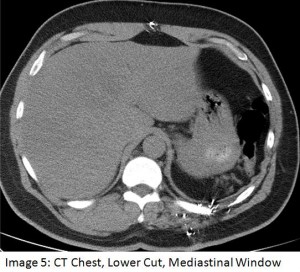
A 61 year old man was referred to the pulmonary service for an abnormal pulmonary function test (PFT). The patient was a lifelong smoker and had symptoms suggestive of obstructive sleep apnea. The PFT showed a mixed obstructive and restrictive defect. The latter abnormality was considered to be out of proportion to the patient’s obesity, hence a chest CT scan was obtained to evaluate for possible parenchymal lung disease (shown below). Past history was significant for hypertension, hyperlipidemia, GERD, and a remote gunshot wound to the back. Medications included irbesartan, simvastatin, omeprazole and combivent.
Work-up revealed a negative bone scan, negative head CT, and a PET scan which showed no abnormal uptake in the thorax. Core needle biopsy of the lesion depicted in Image 3 revealed a chronic mixed inflammatory infiltrate with plasma cells, lymphocytes, endothelial cells and capillaries; tissue resembled parietal pleura with fibrous plaque and malignancy was not identified.