 By Lakshmi Tummala, MD and Todd Cutler, MD
By Lakshmi Tummala, MD and Todd Cutler, MD
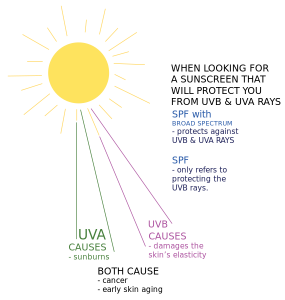
In the spirit of prevention, please wear hats and apply a generous amount of sunscreen while reading this week’s issue of primecuts.
This week the United States Preventive Services Task Force released updated guidelines for cervical cancer screening [1] recommending that women aged 21 to 65 years old, regardless of sexual history, be screened with a PAP smear every three years. For women who wish to lengthen the intervals between screening periods, beginning at age 30, women have the option of undergoing cytology and HPV testing every five years. Both of these recommendations are class A based on evidence showing decreased incidence or mortality of cervical cancer with screening.
Importantly, these recommendations do not apply to women with a history of exposure to diethylstilbestrol, prior cervical cancer or high-grade precancerous lesion, or any form of immunodeficiency. Furthermore, there is no role for screening with HPV testing before 30 years of age, screening at all before 21 years or after 65 years of age (the latter assuming adequate screening to that point) or for screening women after hysterectomy who no longer have a cervix (all grade D).
In comparison to the previous guidelines from 2003, this update acknowledges the higher rate of false positives with HPV testing and the associated risks. It also clearly suggests a time to initiate screening based on patterns of HPV infection with the intent to reduce harm, as management of a cervical lesion does have potentially adverse health consequences for women, especially in pregnancy. Lastly, the authors note that the change from annual screening to every three years may translate into decreased contact between young women and their healthcare providers, and that other routine preventive healthcare measures should not be compromised as a result. We wait to see how these new recommendations will change our clinic practice.
Traditionally, patients with alcoholic cirrhosis have been considered to be at significantly higher risk of developing hepatocellular carcinoma (HCC) than the general population and routine imaging is generally recommended for screening purposes [2] although the US Preventive Services Task Force has no recommendation regarding HCC screening in alcoholic cirrhosis. Both the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver recommend that patients with alcoholic cirrhosis suggest that patients be screened with ultrasound or CT scan every six months [3].
Despite this, however, there have been no randomized clinical trials evaluating the impact of regular screening for HCC on patients with alcoholic cirrhosis. This is, in part, because of widely disparate estimates of the overall incidence of HCC in patients with alcoholic cirrhosis which, in different studies, have ranged from 1% to 16% over five years [4,5].
A publication out of Denmark this week investigated the incidence of HCC in patients with alcoholic cirrhosis [6]. A national registry was used to evaluate all patients identified in the health care system as having alcoholic cirrhosis without underlying viral hepatitis. Since, during this time, no national screening guidelines existed for alcoholic cirrhosis, these patients were monitored over a period without standardized surveillance. The primary outcomes were incidence of HCC and overall mortality.
Of 8,482 patients evaluated, 169 (2.0%) were diagnosed with HCC – a number that increased slightly over time. The risk at five years was to be about 1%. Survival after diagnosis was short with a median time of 97 days for localized HCC and 37 days for nonlocalized HCC. Of the same group of patients, 5,734 (67.6%) died during the study period and 43.7% died within five years of diagnosis. Only about 1.8% of the total deaths in the population were attributable to HCC.
While not an insignificant percentage, the authors suggest that it is unlikely that any national surveillance program will have any significant effect on mortality in patients with alcoholic cirrhosis. This is based on the believe that an annual risk of greater than 1.5% is needed for a mortality benefit to be gained for screening for HCC. The authors argue that this study is likely generalizable to other populations of alcohol cirrhosis and may inform future guidelines regarding screening for HCC in patients with alcoholic cirrhosis [7].
While a role for zidovudine in preventing perinatal transmission of HIV has been firmly established, this week, the NEJM published a study looking at evidence for improved efficacy with combination anti-retroviral therapy [8] – a trend already in practice for some high-risk populations.
Starting in 2004, subjects were recruited primarily from Brazil and South Africa; mothers and infants were excluded if they had received any ARVs besides zidovudine. 1745 infants were enrolled within 48 hours after birth to one of three arms: zidovudine alone, zidovudine plus nevirapine, or zidovudine plus nelfinavir and lamivudine. They were tested for HIV viral loads at birth and then again at multiple intervals with a primary end point of intrapartum HIV infection at three months. Infants found to be infected in utero (positive test at birth) were excluded from study analysis; those found to have an intrapartum infection (positive test after previous negative test) were subsequently withdrawn from the study in order to initiate HIV treatment. Breast-feeding was discouraged, with less than one percent of moms doing so by two weeks post-partum.
There was no difference in the rates of in utero transmission of HIV among the three groups. At three months, infants who received zidovudine alone had a higher rate of intrapartum transmission (4.8%) than infants who received two drugs (2.2%) or three drugs (2.4%). Overall transmission of HIV at almost nine months of follow-up showed a similar trend, with 11.0% of the infants in the zidovudine-alone group carrying the diagnosis, versus 7.1% in the zidovudine/nevirapine group and 7.4% in the zidovudine/nelfinavir/lamivudine group. There was no difference in mortality rates among the three groups. Infants who received three anti-retrovirals had significantly higher rates of neutropenia than the one- or two-drug infant groups (this neutropenia, along with anemia, comprised most of the documented adverse events).
Overall rates of transmission were lower than initially projected, but the differences between groups are still impressive and statistically significant. By self-report, these patients had an impressive 96% adherence rate, which may be higher than can be realistically expected in future applications. On analysis, there were no significant differences in resistance patterns between the groups, also note that 9% of the mothers were found to be co-infected with syphilis, though the impact of this on HIV infectivity was not explored by the authors. In conclusion, it seems that with the simple addition of one drug, we have the potential to really decrease the incidence of intrapartum HIV infection without the cost of significantly increased adverse health effects.
Lakshmi Tummala, MD is a Chief Resident at NYU Langone Medical Center
Dr. Todd Cutler is also a Chief Resident at NYU Langone Medical Center and an associate editor for Clinical Correlations
Image Coutesy of Wikimedia Commons
References:
[1] Moyer et al. Screening for cervical cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2012 Jun 19;156(12):880-91. Available from: http://annals.org/article.aspx?articleid=1183214&atab=7
[2] Sherman M. Hepatocellular carcinoma: screening and staging. Clin Liver Dis. 2011;15:323-34, vii-x. Available from: http://www.liver.theclinics.com/article/S1089-3261(11)00004-3/pdf
[3] Bruix et al. Management of hepatocellular carcinoma: an update. Hepatology. 2011 Mar;53(3):1020-2. Available from: http://www.aasld.org/practiceguidelines/Documents/Bookmarked%20Practice%20Guidelines/HCCUpdate2010.pdf
[4] Toshikuni et al. Comparison of outcomes between patients with alcoholic cirrhosis and those with hepatitis C virus-related cirrhosis. J Gastroenterol Hepatol. 2009 Jul;24(7):1276-83. Available from: http://onlinelibrary.wiley.com/doi/10.1111/j.1440-1746.2009.05851.x/pdf
[5] Fleming et al. All-cause mortality in people with cirrhosis compared with the general population: a population-based cohort study. Liver Int. 2012 Jan;32(1):79-84. doi: 10.1111/j.1478-3231.2011.02517.x. Available from: http://onlinelibrary.wiley.com./doi/10.1111/j.1478-3231.2011.02517.x/abstract
[6] Jepsen et al. Risk for hepatocellular carcinoma in patients with alcoholic cirrhosis: A Danish nationwide cohort study. Ann Intern Med. 2012 Jun 19;156(12):841-7. Available from: http://annals.org/article.aspx?articleid=1183009
[7] Amy Norton. Study doubts value of liver cancer screening [Internet]. Reuters. 06/19/12. Available from: http://www.reuters.com/article/2012/06/19/us-study-liver-cancer-screening-idUSBRE85I1EP20120619
[8] Nielsen-Saines et al. Three postpartum antiretroviral regimens to prevent intrapartum HIV infection. N Engl J Med. 2012 Jun 21;366(25):2368-79. Available from: http://www.nejm.org/doi/full/10.1056/NEJMoa1108275
