Faculty Peer Reviewed
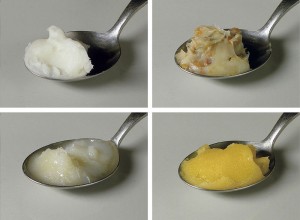
In a move that was almost thirty years in the making, this week the Food and Drug Administration proposed measures that would all-but outlaw artificial trans fats. These artery-clogging, partially hydrogenated oils have long been implicated as a major contributor to heart disease in the United States. Their removal from the U.S. food industry could prevent as many as 20,000 heart attacks and 7,000 deaths from heart disease each year, according to data cited by the FDA. While efforts to limit trans-fats have increased tremendously in recent years, they continue to lurk in many popular (and some would argue, delicious) food products such as frozen pizzas, packaged pies, and microwave popcorn. Although this week’s announcement was viewed as a major food policy victory, nutritionists continue to warn that winning the battle against trans-fats shouldn’t distract from the war against saturated fats. Speaking of tough battles, this week in the medical literature, new breakthroughs were made in the fight against many chronic diseases.
This week in Lancet, the LONESTAR investigators compared the effectiveness of sofosbuvir and ledipasvir fixed-dose combination with and without ribavirin in both treatment-naïve and previously treated patients with genotype-1a and 1b hepatitis C virus (HCV) infection [1]. Currently, protease-inhibitors in combination with interferon injections are the standard of care for treating HCV infection. Interferon treatment, however, is associated with a high number of adverse effects, many of which lead to treatment cessation. Sofosbuvir, a nucleotide analogue inhibitor of an HCV polymerase, and ledipasvir, a potent NS5A inhibitor with antiviral activity against HCV genotypes 1a and 1b, are two new HCV medications that have only been studied in a combination therapy trial once prior [2].
This open label, randomized, Phase 2 trial, involved 100 adult patients with HCV at a single U.S. medical center. The patients were divided into two cohorts, A and B, with cohort A (n=60) composed of treatment naïve, noncirrhotic patients, and cohort B (n=40) composed of patients with treatment failure after receiving a protease inhibitor regimen. In cohort B, 55% of patients had compensated cirrhosis (defined as the absence of ascites, encephalopathy, or history of variceal hemorrhage) and most were demonstrated non-responders to protease inhibitor regimens (68%). Within the cohorts, patient’s baseline characteristics were similar. In cohort A, patients were randomized in equal ratios to receive either 8 weeks of sofosbuvir and ledipasvir (group 1), 8 weeks of sofosbuvir and ledipasvir with ribavirin (group 2), or 12 weeks of sofosbuvir and ledipasvir (group 3). In cohort B, patients were randomized in a 1:1 ratio to either 12 weeks sofosbuvir and ledipasvir (group 4), or 12 weeks of sofosbuvir and ledipasvir with ribavirin (group 5). The primary endpoint was sustained virological response 12 weeks after treatment (SVR12) and all analysis was performed according to the intention-to-treat principle.
For cohort A, SVR 12 was reached by 95% of patients in group 1, 100% in group 2, and 95% in group 3 (n = 20, 21, 19 respectively). In cohort B, SVR12 was achieved in 95% of group 4 and 100% of group 5 (n = 19 and 21 respectively). SVR12 was achieved in these patients regardless of treatment history, presence or absence of cirrhosis, or race which were all previously negative predictors of response. Of the 100 patients in the study, no patients had serologic breakthrough during treatment and only two experienced a virologic relapse following treatment. The vast majority of patients (90%) achieved undetectable levels of quantifiable HCV RNA by week 2 of the study. Overall, adverse events were mostly considered mild and were more common in the groups receiving ribavirin as a part of their therapy. The most common were nausea, anemia, headache and upper respiratory tract infections.
This study had its share of limitations, including small sample size and lack of powering for group comparison, being only a single-center trial, and lacking blinding as a part of the methodology. Despite this, the study offers exciting results for the future of HCV therapy, especially with regards to patient’s that have experienced treatment failure or in those concerned with potential drug side effects from current therapies. This trial is more importantly, one of the first to demonstrate a profound effect in both treatment naïve patients in addition to patients with failed treatment and compensated cirrhosis. Large-scale multicenter studies are currently underway, and hopefully sofosbuvir plus ledipasvir will prove to be an effective HCV treatment on a larger scale.
Moving on to hematology, the current standard of care for many patients with chronic myeloid leukemia (CML) includes initial treatment with imatinib, a first generation tyrosine-kinase inhibitor (TKI). Despite great early response rates, up to 40% fail treatment as they either develop disease resistance (often due to BCR-ABL kinase domain mutations) or unacceptable side effects during the often lengthy treatment periods. Second generation TKIs are subsequently ineffective in up to 50% of patients who fail imatinib. The effect of ponatinib, a novel tyrosine-kinase inhibitor, in Philadelphia chromosome positive leukemias was examined in this week’s New England Journal of Medicine [3].
This open label, multinational, phase 2 trial involved 444 patients with either CML or Ph-positive ALL all of whom had been previously treated with a second generation TKI or had inherent resistance. Patients were split into cohorts depending their specific disease (chronic phase CML, accelerated phase CML, blast phase CML, or Ph-positive ALL), and whether they had developed resistance to, or unacceptable side effects from second generation TKIs. In addition, patients with the T315I mutation (which confers resistance to all other approved TKIs) were also identified prior to the study. The primary endpoint studied was a major cytogenic response at anytime in the first 12 months in chronic CML patients, and a major hematologic response anytime during the first 6 months in all other patients.
Of the 267 with chronic phase CML 56% were shown to have a major cytogenic response, most pronounced in younger, less heavily pretreated patients. In accelerated phase CML major cytogenic response was seen in 39%, 31% in blast phase CML, and 47% in Ph-positive ALL. In chronic phase CML, 12-month survival (a secondary endpoint), was above 80%. While the effect of ponatinib in resistant CML looks promising there appears to be a dangerous association with arterial thrombotic events. In this study 8.9% of patients had arterial thrombotic events, of which 2.9% were treatment related. Of note, ponatinib recently received a black-box warning for arterial thrombotic events and a major randomized trial assessing ponatinib versus imatinib was recently halted due to an accumulating number of these events. Data from the trial published this week suggests risk is highest in those patient with pre-existing ischemic risk factors, however it remains to be seen whether ponatinib will be the drug of choice in treating CML and other Ph-positive tumors or these adverse events will outweigh any benefit incurred.
In the Annals this week, investigators proposed the utilization of a home score for streptococcal pharyngitis [4]. With over 12 million annual outpatient visits to providers for pharyngitis in the U.S., accurate diagnosis has significant implications not only on the patient’s well being, but on associated costs. As physical exam alone does not usually help clinicians make a final diagnosis of group A streptococcal (GAS) pharyngitis, scoring systems such as the Centor score (fever, absence of cough, tonsillar exudates, tender anterior cervical lymphadenopathy) and McIssac score (Centor score plus age) have guided treatment and testing decisions. This retrospective analysis included 71,776 patients greater than 15 years of age, who presented to nationally based CVS MinuteClinics with the chief complaint of sore throat. Providers at these MinuteClinics followed the Strep Pharyngitis Algorithm from the Institute for Clinical Systems Improvement, and after collecting pertinent information all patients with pharyngitis were tested for GAS. The patients included were divided into a derivation set (n = 48, 089) and a validation set (n = 23,687) for the scoring system.
The home score used in this study included the two Centor score criteria that patients could reliably identify: fever and absence of cough, as well as age from the McIssac Score. A fourth, previously validated variable that reflects disease incidence—the recent local proportion positive, or RLPP—was also included. With the score ranging from 0-100, based on the data collected if a patient’s calculated home score was only 10, it translated to a negative predictive value of 90%. This was confirmed using the validation cohort, in which a score of 10 was associated with an 87% NPV. Using this cutoff, up to 230,000 visits for GAS pharyngitis could be saved. Despite the prevented visits, however, 8500 patients who would have been treated using the Centor score would go without antibiotics. While GAS pharyngitis is usually self-limited, complications of untreated disease such as rheumatic fever or abscess formation are still possible, stressing the importance of appropriate triage (the authors suggest with a telephone system) and follow-up for any patients that appear ill. While there is always some inherent risk associated with home testing, this scoring system has utility to help predict a non-GAS illness and could save hundreds of thousands of unnecessary doctor visits annually.
The adverse respiratory effects of acute beta-blocker exposure in asthma were analyzed in Chest this week [5]. This systematic review and meta-analysis of randomized, controlled trials aimed to determine the risk of bronchoconstriction in acute exposure to both selective (beta-1) and non-selective beta-blockers. The analysis included 32 blinded, randomized, placebo-controlled trials, of which 16 assessed selective beta-blockers, 6 evaluated non-selective beta-blockers, and 10 studies looked at both. The most common beta-blockers studied were metoprolol, atenolol, and propranolol. Heterogeneity was evaluated using the I2 statistic.
Acute selective beta-blocker exposure was associated with an average change in the forced expiratory volume in one second (FEV1) of -6.9% (95%CI -8.5 to -5.2). Also a decrease in FEV1 > 20% was seen in 1 out of every 8 patients (P=0.03). The respective values for acute non-selective beta blockers were -10.2% (95%CI -14.7 to -5.6) and 1 of 9 patients (P=0.02). Response to beta-2 agonist administration was also shown to be greater after selective compared to non-selective beta-blocker administration (crude mean FEV1 response +16% and -0.7%, respectively). The trials included in this meta-analysis used different medications at varying doses, however. While the message that one must be careful in acutely administering beta-blockers to patients with asthma was reinforced, especially with regard to non-selective beta-blocker use, from the results of this meta-analysis no solid conclusions can be drawn with regards to risks associated with individual beta-blockers or doses.
Other interesting articles this week:
In JAMA, Vinden et al. studied whether surgeons operating the night before led to increased complications of daytime elective laparoscopic cholecystectomies [6]. Overall they found no differences in the complication rate of surgeons that operated the night before (from 12am to 7am) and those that did not.
The risk of hypotension in adult patients with BPH initiating treatment with tamsulosin was reviewed in the British Medical Journal [7]. This population based, retrospective cohort study found that there was an increased risk of hypotension requiring hospitalization in patients starting tamsulosin, especially in the first eight weeks of treatment.
Lastly, in Circulation this week, racial and ethic differences in dyslipidemia patterns were reviewed [8]. The main groups studied, were Asian Americans, Mexican Americans, and African Americans compared to non-Hispanic whites. Authors found that, except for African Americans, minority groups were more likely to have high triglyceride/low HDL –C dyslipidemia.
Dr. Sherif Shoucri is a 1st year resident at NYU Langone Medical Center
Peer reviewed by Gregory Schrank, MD, Contributing Editor, Clinical Correlations
Image courtesy of Wikimedia Commons
References:
1. Lawitz E et al. Sofosbuvir and ledipasvir fixed-dose combination with and without ribavirin in treatment naïve and previously treated patients with genotype 1 hepatitis C virus infection (LONESTAR): an open label, randomized, phase 2 trial. Lancet. Early online publication 5 Nov 2013. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(13)62121-2/abstract
2. Gane EJ, Stedman CA, Hyland RH, et al. ELECTRON: all-oral sofosbuvir-based 12-week regimens for the treatment of chronic HCV GT 1 infection. 48th annual meeting of the European Association for the Study of the Liver; Amsterdam, The Netherlands; April 24–28, 2013.
3. Cortes JE et al. A Phase 2 Trial of Ponatinib in Philadelphia Chromosome-Positive Leukemias. N Engl J Med. 2013;369:1783-96. http://www.nejm.org/doi/full/10.1056/NEJMoa1306494
4. Fine AM et al. Participatory Medicine: A Home Score for Streptococcal Pharyngitis Enabled by Real-Time Biosurveillance. Ann Intern Med. 2013;159:577-583. http://annals.org/article.aspx?articleid=1763228
5. Morales DR et al. Adverse respiratory effect of acute beta-blocker exposure in asthma: a systematic review and meta-analysis of randomized controlled trials. Chest. Early Online Publication 7 Nov 2013. http://journal.publications.chestnet.org/article.aspx?articleid=1767055
6. Vinden C et al. Complications of daytime elective laparoscopic cholecystectomies performed by surgeons who operated the night before. JAMA. 2013;310(17):1837-1841. http://jama.jamanetwork.com/article.aspx?articleid=1764050
7. Bird ST et al. Tamsulosin treatment for benign prostatic hyperplasia and risk of severe hypotension in men aged 40-85 years in the United States: risk window analyses using between and within patient methodology. BMJ. 2013;347:f6320. http://www.bmj.com/content/347/bmj.f6320
8. Frank ATH et al. Racial/Ethnic Differences in Dyslipidemia Patterns. Circulation. Early online publication 5 Nov 2013. http://circ.ahajournals.org/content/early/2013/11/04/CIRCULATIONAHA.113.005757.abstract