Peer Reviewed
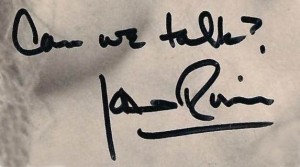
In sports news this week, the Seahawks crushed the Packers, 36-16, in the NFL season opener as Aaron Rodgers “played scared” against the Seahawks defense led by Richard Sherman, according to the Milwaukee Journal Sentinel. In actual news, the U.S. military continued airstrikes against ISIS in Iraq and clashes between Ukrainian troops and pro-Russian militants continued in Eastern Ukraine despite a ceasefire agreement. A federal judge ruled that BP should be fined $18 billion for “profit-driven decisions and willful misconduct” in the 2010 Deepwater Horizon oil spill in the Gulf of Mexico. And finally, Joan Rivers died after an outpatient surgery on her vocal cords. She had once written that she wanted her funeral to be “a huge showbiz affair with lights, cameras, action,” which it apparently lived up to on Sunday.
This week in the wide world of medicine, important studies were published on diet and weight loss, and treatment regimens for multiple myeloma.
Comparison of diet strategies for weight loss and cardiovascular risk. Is a low-carbohydrate or low-fat diet better?
Two major studies were published this week comparing diet strategies for weight loss, coming to slightly different conclusions. A randomized control trial published in Annals of Internal Medicine found a low-carbohydrate diet to be superior to a low-fat diet for weight loss and cardiovascular risk reduction. [1] The study randomized 148 obese men and women without diabetes or coronary artery disease to a low-carbohydrate diet or low-fat diet. Nearly 90% of the participants were women, 50% were black, the mean age was 47, and mean body mass index was 35. Those in the low-carbohydrate group were instructed to maintain an intake of digestible carbohydrate of less than 40g/dL, while those in the low-fat group were told to maintain less than 30% of their daily energy intake from fat and 55% from carbohydrate based on National Cholesterol Education Program guidelines. Neither diet had a specific calorie goal. About 80% of participants completed the study through one year of follow up. Caloric intake was slightly, but not significantly lower in the low-carbohydrate group, and not surprisingly, those in the low-carbohydrate group ate significantly less carbs and more fat than those in the low-fat group. At 3, 6, and 12 month follow up, the low-carbohydrate group had significantly improved weight loss (mean weight loss at 1-year: 5.3kg vs. 1.8kg, weight loss difference -3.5kg, 95% CI: -5.6 to -1.4kg), total to HDL cholesterol ratio, triglycerides, c-reactive protein level, and estimated 10-year cardiovascular risk compared to the low-fat group. Though specific cardiovascular outcomes were not assessed, this new evidence suggests that a low-carbohydrate diet may be more effective than a low-fat diet for weight loss and cardiovascular risk reduction.
In contrast to these findings, a meta-analysis appearing in JAMA this week found similar weight loss effects for multiple diet strategies when compared to no diet or an alternative. [2] The study assessed branded diets (e.g. Atkins, Zone, LEARN) or “brand-like” diets, which were judged to be similar to a branded diet but did not reference a specific brand. The study included 48 randomized trials with 7,286 overweight or obese individuals. Average age was 46 and mean BMI was 24. Diets were grouped into low-carbohydrate, low-fat, and moderate macronutrient (i.e. balanced fat and carbs) categories, although most of the included studies assessed low-carbohydrate diets. All diet types were superior to no diet for weight loss at 6-month follow up. Low-carbohydrate diets resulted in a median weight loss difference of 8.73kg (95% CI 7.27-10.20kg) at 6 months compared to no diet or an alternative, while low-fat diets resulted in a 7.99kg (95% CI 6.01-9.92kg) 6-month weight loss difference compared to controls. The difference was not statistically significant, although low-carbohydrate diets did result in statistically greater weight loss than the moderate macronutrient diet class. The authors conclude, however, that “the differences were small and unlikely to be important for those seeking weight loss” and “supports the practice of recommending any diet that a patient will adhere to in order to lose weight.”
Aspirin following anticoagulation in patients with unprovoked venous thromboembolism
Patients with unprovoked venous thromboembolism (VTE) are at high risk of recurrence even after completing a course of anticoagulation (~10% in the first year and ~5% per year thereafter), however, extending anticoagulation increases the cumulative risk of bleeding. Two trials previously published in The New England Journal of Medicine (WARSAFA and ASPIRE) in 2012 found a decreased rate of recurrence of VTE with aspirin as compared to placebo, however, the finding was not statistically significant in the ASPIRE trial. Results combining individual patient data from the two trials were published ahead of print in Circulation this week, with the rationale that the prior studies were “underpowered to detect moderate treatment effects for particular outcomes or subgroups.” [3] The trials had similar design—each randomized patients with a first unprovoked VTE event to 100mg of aspirin vs. placebo after completing 6 to 18 months of anticoagulation. Follow up was 2 years in the WARSAFA trial and 4 years in the ASPIRE trial. Patients in the WARSAFA trial were older, more likely to be male and smokers, and less likely to be obese. In combined data from 1,224 patients, the rate of recurrence of symptomatic VTE was 5.1% per year in the aspirin group vs. 7.5% per year in the placebo group (HR: 0.68, 95% CI: 0.51-0.90, number needed to treat (NNT): 42). The effect was similar for PE and DVT. There was no difference in fatal PE (2 in each group). The rate of “clinically relevant” bleeding was 1.1% vs. 0.7% per year in the Aspirin vs. placebo group, which was non-significant. The relative effect of aspirin was similar across subgroups, however, the absolute benefit of aspirin was greater in subgroups at higher risk for VTE, including men (NNT 31), patients over 65 (NNT 19), and within the first year of treatment (NNT 18). Not surprisingly, aspirin also reduced the risk of major vascular events. While the effect of aspirin on recurrent VTE is much less than warfarin (relative risk reduction ~30-40% vs. 80%), the authors recommend “aspirin should be strongly considered” in patients with unprovoked VTE who would not otherwise be on anticoagulation.
High-dose chemotherapy and autologous stem cell transplantation vs. a novel consolidation regimen as initial therapy for multiple myeloma
Recent years have seen major advances in treatment for multiple myeloma with new immunomodulatory drugs and proteasome inhibitors showing promise in patients with relapsed or refractory disease. This has called into question the current standard of care for initial therapy in patients under 65; high-dose chemotherapy with autologous stem cell transplantation, which carries significant morbidity and mortality. This week, a randomized trial comparing high-dose chemotherapy (melphalan) and autologous stem cell transplantation (SCT) vs. a consolidation regimen of melphalan-prednisone-lenalidomide (MPR; “R” for Revlimid, the trade name for lenalidomide, an immunomodulatory agent) was published in The New England Journal of Medicine. [4] The study was a complicated design—patients with newly diagnosed multiple myeloma under 65 were randomized to one of the above treatments for consolidation therapy following induction, and later randomized again in order to additionally study lenalidomide maintenance therapy. Important exclusion criteria were age>65, life expectancy< 6 months, high disability score, neutrophil count <1500, platelets<75k, and poor cardiac, pulmonary, or renal function (CrCl<30). A total of 402 patients were enrolled, however, only 273 patients remained at the time of randomization to SCT vs. MPR. With regards to the primary endpoint of median progression-free survival, high-dose chemotherapy and SCT was superior to MPR consolidation therapy (43.0 months vs. 22.4 months; HR for progression or death 0.44, 95% CI: 0.32 to 0.93). In addition, 4-year overall survival was 81.6% in the high-dose chemotherapy and SCT group vs. 65.3% in the MPR group. The superiority of high-dose chemotherapy and SCT was despite significantly higher rates of neutropenia, thrombocytopenia, infections, gastrointestinal, and systemic events. As a result, high-dose chemotherapy with stem-cell transplantation will remain the standard of care for initial treatment of multiple myeloma in patients under 65 who can tolerate it.
Also in the journals this week…
Carvedilol vs. metoprolol succinate for heart failure
In a Danish cohort of 11,664 patients with heart failure with reduced ejection fraction (<40%) and median follow up of 2.4 years, there was no difference in mortality between patients on carvedilol vs. metoprolol (HR: 0.99, 95% CI: 0.88 to 1.11) after adjustment using a propensity score that included 126 variables. [5]
Limited long-term evidence on bariatric surgery
A systematic review appearing in JAMA looking at outcomes of bariatric surgery found few studies with greater than 2 years of follow up and more than 80% patient retention, cautioning that the long-term risks and benefits of certain types of bariatric surgery have still yet to be fully characterized. [6]
NAC for prevention of COPD exacerbations
A randomized control trial from China appearing in CHEST found high-dose N-acetylcysteine reduced COPD exacerbation frequency compared to placebo in a subgroup of high-risk patients already on standard therapies for COPD. [7]
Impaired responsiveness to Plavix in diabetics
An in vitro study published in the Journal of the American College of Cardiology found that patients with diabetes and coronary artery disease had greater residual platelet activity following a loading dose of clopidogrel compared to non-diabetics with coronary artery disease after performing multiple pharmacokinetic and pharmacodynamics assessments. [8]
Dr. Vaughan Touhy is a 2nd year resident at NYU Langone Medical Center
Peer reviewed by Gregory Schrank, MD, Contributing Editor, Clinical Correlations
Image courtesy of Wikimedia Commons
References:
1. Bazzano LA et al. Effects of Low-Carbohydrate and Low-Fat Diets: A Randomized Trial. Annals of Internal Medicine. 2014; 161: 309-318. doi:10.7326/M14-0180. http://annals.org/article.aspx?articleid=1900694
2. Johnston, BC et al. Comparison of Weight Loss Among Named Diet Programs in Overweight and Obese Adults: A Meta-Analysis. JAMA. 2014;312(9):923-933. doi:10.1001/jama.2014.10397. http://jama.jamanetwork.com/article.aspx?articleid=1900510
3. Simes J et al. Aspirin for the Prevention of Recurrent Venous Thomboembolism: The INSPIRE Collaboration. Circulation. 2014. DOI: 10.1161/CIRCULATIONAHA.114.008828. http://circ.ahajournals.org/content/early/2014/08/12/CIRCULATIONAHA.114.008828.abstract
4. Palumbo A et al. Autologous Transplantation and Maintenance Therapy in Multiple Myeloma. NEJM. 2014; 371: 895-905. doi: 10.1056/NEJMoal402888. http://www.nejm.org/doi/full/10.1056/NEJMoa1402888
5. Pasternak B et al. Association of Treatment with Carvedilol vs Metoprolol Succinate and Mortality in Patients with Heart Failure. JAMA Inern Med. Published online August 31, 2014. doi:10.1001/jamainternmed.2014.3258. http://archinte.jamanetwork.com/article.aspx?articleid=1899761
6. Puzziferri N et al. Long-term Follow-up After Bariatric Surgery: A Systematic Review. JAMA. 2014;312(9):934-942. doi:10.1001/jama.2014.10706. http://jama.jamanetwork.com/article.aspx?articleid=1900516
7. Hoi NT et al. Benefits of High-Dose N-Acetylcysteine to Exacerbation-Prone Patients With COPD. Chest. 2014;146(3):611-623. doi:10.1378/chest.13-2784. http://journal.publications.chestnet.org/article.aspx?articleID=1873029
8. Angiolillo DJ et al. Impaired Responsiveness to the Platelet P2Y12 Receptor Antagonist Clopidogrel in Patients with Type 2 Diabetes and Coronary Artery Disease. J Am Coll Cardiol. 2014;64(10):1005-1014. doi:10.1016/j.jacc.2014.06.1170