Peer Reviewed
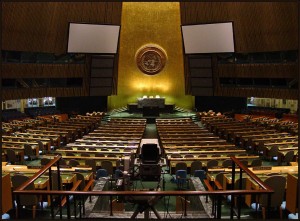
Pleasant fall weather was not the only visitor to New York last week. Major global dignitaries descended on midtown to convene the 69th Session of the General Assembly of the United Nations. President Obama made an appearance to seek support in the fight against ISIS militants. In local news, New Yorkers learned that Mayor De Blasio may have played a role in the death of a beloved Staten Island groundhog earlier this year by dropping her inadvertently [1]. The article notes “Mr. de Blasio’s dexterity has come into question in recent days. Last week, while playing first base at a softball game against the City Council, the mayor flubbed several catchable throws that came his way.” Lastly, Rosh Hashanah, the Jewish New Year, was celebrated. Shanah Tovah, everyone.
In medical news, both the WHO and the CDC released updates and projections for the Ebola epidemic.
Ebola Update from the WHO:
Writing in the New England Journal of Medicine, the WHO updates descriptive statistics from Guinea, Liberia, Nigeria and Sierra Leone [2]. The most common symptoms in cases were fever (87%), fatigue (76%) and GI complaints. Characteristic hemorrhagic symptoms were only seen in up to 5.7%, most frequently bloody stool, but 18% had “unexplained bleeding.” Case-fatality rate was 71%. Mean incubation time was 11.4 days.
From a public health perspective, there are worrisome findings. The mean time from symptom onset to hospitalization was 5 plus or minus 4.7 days, a finding that was no different for healthcare workers. The presence of symptomatic patients in the community may largely drive the rapid doubling time of the epidemic: 15.7-30.2 days. As of September 21, there are 6,263 cases [3]. Without intervention, >20,000 cases are expected by November 2, 2014.
Additionally, the R0, the measure of how many new infections will arise from a primary case in an uninfected population, is estimated at 1.71-2.02 for the hardest hit countries. This means that interventions need to cut transmission in half to bring the disease under control.
That said, the authors remind us that these R values alone are not severe. For context, SARS was estimated to have an R of 3 early in its course, and was contained with basic infection control practices [4; 5]. (Admittedly, SARS was a very different disease in a very different setting.) To this end, the CDC reminds us that isolation is paramount in controlling the epidemic…
Is the End in Sight?
In their Morbidity and Mortality Weekly Report, the CDC reports on its Ebola Response model in Liberia and Sierra Leone, the two hardest-hit countries [6]. The model classifies cases into one of three isolation categories: hospitalized in an Ebola treatment unit (ETU), isolated at home or not isolated at all. The risk of disease transmission based on isolation status is estimated, accounting for a mean incubation period of six days and infectious period lasting six days. Two models of control are offered. The first scenario ends the epidemic by mid-January 2015 if a larger percentage of patients were isolated starting in late August, with gradual increases in isolation so that by late December, 25% of cases are in ETUs and 45% are isolated at home. The second model accounts for delaying interventions. In this model, 70% of patients would need to be in ETUs to effectively control the disease. But, for every 30 days passed without increasing the percentage of patients in ETUs, the number of new daily cases will triple.
What you may find most unsettling is the reference to “substantial underreporting.” The CDC offers a correction factor of 2.5 for cases in these countries. That means that for every known case, it is assumed that there are likely 2.5 actual cases. Left unchecked, we can expect 1.4 million cases by January 2015.
Polyethylene Glycol vs Lactulose for Hepatic Encephalopathy
In JAMA Internal Medicine, investigators reevaluated lactulose as the mainstay of treatment for hepatic encephalopathy (HE) [7]. This randomized trial compared polyethylene glycol (PEG) to lactulose in 50 cirrhotic patients. 25 patients were randomized to each unblinded treatment arm and then treated with either PEG (4L) or lactulose (20-30g at least 3 times a day by mouth or NG tube or 200g by rectum). Demographics and baseline characteristics were similar between treatment cohorts, and patients were primarily of Hispanic ethnicity and white. HE was measured by Hepatic Encephalopathy Scoring Algorithm (HESA) grade. 43% of patients in the PEG group improved to a HESA grade 0 (total resolution of HE) within 24 hours, compared with 8% in the lactulose group. Mean HESA score at 24 hours was lower for those receiving PEG (0.9 vs. 1.6, p = 0.002), and the median time to total resolution was one day for PEG vs. two days for lactulose (p = 0.01).
This is a small study that was conducted at a single center in a largely unblinded fashion. Nonetheless, the results are robust and challenge the core treatment of a common condition.
Which Drug Combinations Have the Highest Risk of Upper GI Bleed?
It is well established that certain medications, such as NSAIDs and aspirin, are associated with an increased risk of upper GI bleed (UGIB). It is suspected that combining these medications with other classes of drugs, such as steroids and SSRIs, is associated with greater risk. In Gastroenterology, investigators conducted a retrospective case series analysis, culling data on UGIB from seven databases in three European countries [8]. 12 classes of drugs were investigated, from common culprits such as antiplatelet and anticoagulation agents to nitrates and calcium channel blockers. The highest-risk monotherapy was nonselective NSAIDs (nsNSAIDs) (IRR 4.27, 95% CI 4.11-4.44) and corticosteroids (IRR 4.07, 95% CI 3.83-4.32). Combining any drugs with nsNSAIDs generally had higher risk (IRR 6.9, 95% CI 5.3-9.1) than combinations with low-dose aspirin (IRR 4.6, 95% CI 3.6-6.0) or COX-2 inhibitors (IRR 4.2, 95% CI 3.0-5.9).
The highest-risk combination was nsNSAIDs with corticosteroids (IRR 12.82, 95% CI 11.17-14.72) and this combination had a relative excess risk due to interaction (RERI) of 5.5 (CI 3.7-7.3). This suggests that there is a synergistic effect of these medications; when combined, they lead to a total risk of UGIB that is greater than the sum of their individual risks. Similarly high risks and synergistic effects were observed for nsNSAIDs with aldosterone antagonists (RERI 4.5) and low-dose aspirin with corticosteroids (RERI 2.54).
This study should encourage clinicians to keep a close watch on polypharmacy in their patients. NSAIDs, while common and readily available, possess real risks that are magnified when combined with other drugs.
In other news…
6 vs 12 Months of Dual Antiplatelet Therapy (DAPT) after Second Generation Drug Eluting Stents (DES)
A randomized trial of 1399 patients demonstrates that six months of DAPT after second generation DES placement in low-risk patients is non-inferior to 12 months with respect to major cardiovascular outcomes (cardiac death, MI, CVA, stent thrombosis) or catastrophic bleeding [9].
Speaking of Placing Stents… Patient Perceptions of Percutaneous Coronary Intervention (PCI) for Stable Coronary Artery Disease (CAD)
A study found that patients undergoing PCI for stable CAD had poor understanding of the benefits of the procedure, with 90% believing it will extend life and 88% expecting it would prevent future MIs, despite established evidence suggesting otherwise. Only 1% of patients reported symptom relief as the only benefit. The study, which took place at 10 US academic centers, found that patient perceptions varied by hospital [10].
Follow-Up Testing for Hepatitis C
A large, multi-center retrospective analysis revealed that less than 61% of patients who screened positive for Hepatitis C with an antibody test had a follow-up viral load, which suggests that over a third of patients were not evaluated for treatment [11]. The strongest predictor of having a timely viral load checked was high income.
Dr. Asher Schranz is a 2nd year resident at NYU Langone Medical Center.
Peer Reviewed by Cilian J. White, M.D., Internal Medicine Resident, NYU Langone Medical Center
Image courtesy of Wikimedia Commons
References
1. Flegenheimer M. (2014, September 25). De Blasio’s Fault or Not, Fatal or Not, Groundhog Had an Early Fall. The New York Times. Retrieved September 28, 2014, from http://www.nytimes.com/2014/09/26/nyregion/a-groundhog-day-whodunit-the-mystery-of-chucks-death.html
2. WHO Ebola Response Team. Ebola Virus Disease in West Africa — The First 9 Months of the Epidemic and Forward Projections. New England Journal of Medicine. 2014; Epub ahead of print. http://www.nejm.org/doi/full/10.1056/NEJMoa1411100
3. CDC: 2014 Ebola Outbreak in West Africa. Retrieved September 27, 2014, from http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/index.html
4. Wallinga J, Teunis P. Different Epidemic Curves for Severe Acute Respiratory Syndrome Reveal Similar Impacts of Control Measures. American Journal of Epidemiology. 2004;160(6):509–516. http://aje.oxfordjournals.org/content/160/6/509.long
5. Weinstein RA. Planning for Epidemics – The Lessons of SARS. New England Journal of Medicine. 2014;350(23):2332–2334. http://www.nejm.org/doi/full/10.1056/NEJMp048082
6. Meltzer M, Atkins CY, Santibanez S, et al. Estimating the Future Number of Cases in the Ebola Epidemic — Liberia and Sierra Leone, 2014–2015. MMWR Supplement. 2014;63(3):1–14. http://www.cdc.gov/mmwr/preview/mmwrhtml/su6303a1.htm?s_cid=su6303a1_w
7. Rahimi RS, Singal AG, Cuthbert JA, Rockey DC. Lactulose vs Polyethylene Glycol 3350-Electrolyte Solution for Treatment of Overt Hepatic Encephalopathy: The HELP Randomized Clinical Trial. JAMA Internal Medicine. 2014; Epub ahead of print. http://archinte.jamanetwork.com/article.aspx?articleid=1906996
8. Masclee GMC, Valkhoff VE, Coloma PM, et al. Risk of Upper Gastrointestinal Bleeding From Different Drug Combinations. Gastroenterology. 2014;147(4):784–792.e9. http://www.gastrojournal.org/article/S0016-5085(14)00768-9/abstract
9. Colombo A, Chieffo A, Frasheri A, et al. Second Generation Drug-Eluting Stents Implantation Followed by Six Versus Twelve-Month – Dual Antiplatelet Therapy- The SECURITY Randomized Clinical Trial. Journal of the American College of Cardiology. 2014; Epub ahead of print. http://content.onlinejacc.org/article.aspx? articleid=1906459
10. Kureshi F, Jones PG, Buchanan DM, Abdallah MS, Spertus JA. Variation in patients’ perceptions of elective percutaneous coronary intervention in stable coronary artery disease: cross sectional study. BMJ. 2014;349(sep08 8):g5309–g5309. http://www.bmj.com/content/349/bmj.g5309
11. Spradling PR, Tong X, Rupp LB, et al. Trends in HCV RNA Testing Among HCV Antibody–Positive Persons in Care, 2003–2010. Clinical Infectious Diseases. 2014;59(7):976–981. http://cid.oxfordjournals.org/content/early/2014/07/01/cid.ciu509