Peer Reviewed
It is the last admission of your admitting night shift. You are called to assess a pleasant, oriented 65-year-old man with lung cancer and metastases to the bone, liver, and brain. You review his history along with his admission labs and imaging, and you quickly feel confident in your diagnosis of a lobar pneumonia. Relieved, tired, the sun peaking through the call window, you begin to put in his orders. Finally, your last task is to choose adequate venous thromboembolism (VTE) prophylaxis—you hesitate. You know that his current metastatic disease makes him especially susceptible to VTE. But what about his brain metastasis? Is he at an increased risk of spontaneous intracranial bleed? How do you weigh protecting him from VTE against the devastation of intracranial hemorrhage?
ASCO guidelines give a 1A recommendation, for thromboprophylaxis in bed-bound inpatients who have cancer [1]. The incidence of deep vein thrombosis (DVT) or pulmonary embolism in these patients is 10-30%, leading to a nearly 47-fold increase in mortality from VTE compared to the general population [2]. The common choice for prophylaxis in these patients is a low-molecular-weight heparin (LMWH) like enoxaparin, based on extrapolations from data in the ENOXACAN and the CLOT trials [3,4]. However, in brain tumors, should we feel comfortable with these extrapolations? On the one hand, brain tumors are included in a short list of malignancies that are particularly prone to VTE, along with gastrointestinal, lung, gynecological, renal, and hematological cancers [1]. Rates of VTE in high-grade gliomas (the most common primary brain tumor) can range from 15-30%, and as high as 60% post-operatively [2,5,6]. On the other hand, only 27 of 676 patients with primary brain tumors were included in the CLOT trial, and no bleeding data for this specific subgroup was given [3].
You then consider what kind of brain tumor your patient has and its propensity to bleed. In this case, the patient has metastatic lung adenocarcinoma. Brain metastases from melanoma, thyroid cancer, renal cell carcinoma, and choriocarcinoma are traditionally known to pose the greatest baseline risk for spontaneous intracranial bleeding [7]. For your patient, rate of spontaneous intracranial hemorrhage (ICH) from metastatic lung adenocarcinoma appears to be comparatively low [8]. You breathe a little easier.
You then consider alternatives to anticoagulation. Pooled data using varied patient populations with malignancy shows a statistically significant decrease in deep vein thrombosis with the use of mechanical prophylaxis alone. However, this benefit does not extend to a significant reduction in the risk for pulmonary embolism [1]. In several small prospective studies, IVC filters have effectively shown neither a decrease in intracranial bleeds nor improved overall survival [5,6,12] and ACCP guidelines recommend against prophylactic IVC filters. No easy solution there.
You pull up some guidelines. National Comprehensive Cancer Network guidelines state that “intracranial or spinal lesions at high risk for bleeding” are an absolute contraindication to prophylactic or therapeutic anticoagulation. However, there are no further discussions, definitions, or citations on which this recommendation is based [11]. The American Society of Clinical Oncology (ASCO) guidelines meanwhile state that “the presence of an intracranial tumor or brain metastases without evidence of active bleeding is not an absolute contraindication to anticoagulation” [1].
The fact is that limited data exists on the risks and benefits of VTE prophylaxis in the setting of known brain tumors. You are forced to look for related data to help you make your own clinical decision. The question is not unfamiliar. Several small retrospective studies have demonstrated the effectiveness of unfractionated heparin and warfarin as secondary prophylaxis in patients with primary and metastatic brain tumors. Among these is a 1993 study looking at 49 patients with intracranial malignancy and concurrent VTE. Of the 49 patients, only 15 were treated with anticoagulation, and none of those 15 resulted in ICH or other major bleeds [10]. Another retrospective study of 49 patients with primary and metastatic brain tumors matched by malignancy type and location of VTE were divided between two groups based on whether they received anticoagulation or an IVC filter. The two groups had statistically equivalent rates of intracranial bleeds and mortality at 8 weeks [12]. These results seem to indicate that the rate of bleeding on anticoagulation was equivalent to the rate of spontaneous bleeding off anticoagulation. However, the study was limited by size and its retrospective design. Perhaps those chosen for IVC filters were deemed to be at greater clinical risk for ICH to begin with. And again, these studies were all conducted with the question of secondary prophylaxis in patients with VTE.
The randomized placebo-controlled PRODIGE trial was initiated to look specifically at primary VTE prophylaxis in patients with malignant gliomas using the LMWH dalteparin versus placebo for 6 months after initial surgery. Development of objective DVT or PE was the primary endpoint. By 6 months, 11% in the LMWH group versus 17% in the placebo group developed VTE. Though this difference favored prophylaxis with LMWH, it was not statistically significant. Major bleeds were a secondary end-point. All bleeds in this trial ended up being intracranial bleeds, with 5 patients (5%) suffering intracranial bleeds in the LMWH group compared to 1 patient (1.2%) in the placebo group. This difference was also not statistically significant. While the trial seems to show trends toward improved VTE prophylaxis at the cost of increased intracranial bleeds, this Pfizer funded study was ended early because of an “expiration of study medication [with] no further re-supply” [13].
Perhaps most helpful was a recent matched retrospective cohort study by Donato et al. The study compared rates of ICH in patients with metastatic brain tumors and VTE on therapeutic enoxaparin versus matched subjects without VTE not on enoxaparin. Patients on enoxaparin suffered ICH at a rate of 19%, compared to 21% of patients not on anticoagulation, demonstrating no increased risk of ICH for patients with brain tumors while on anticoagulation. Similar rates persisted regardless of whether or not the bleeds were symptomatic or just picked up on imaging. Subgroup analyses also looking at the incidence of ICH based on malignancy type, and demonstrated no difference between anticoagulated versus non-anticoagulated groups. Rather, in this subgroup analysis, rates of ICH in melanoma and renal cell carcinoma in both anticoagulated and non-anticoagulated groups were equal and substantially higher than other types of malignancies such as metastatic lung cancer (HR 3.98; P < 0.001) [8]. Though renal cell carcinoma and melanoma carry the highest risk of intratumoral bleeds, even these malignancies showed no increased risk of bleeding on anticoagulation.
For decades, clinicians have grappled with striking a balance between bleeding and thrombosis. Medicine is a science, replete with cohorts and p-values and confidence intervals. But in questions such as this, science is limited by practicalities that force us to take what sparse data may exist and treat to the best of our clinical intuition. Donato et al. may provide the best foothold to help make this clinical decision. Even therapeutic doses of anticoagulation may not increase the risk of an intracranial hemorrhage even in the malignancies most prone to do so. These findings most closely resemble the brief ASCO statement that “the presence of an intracranial tumor or brain metastases without evidence of active bleeding is not an absolute contraindication to anticoagulation.” But with that, in the early hours of a new morning, we are left to decide what is best for our patient.
Commentary by David Green, MD, PhD, Director Adult Coagulation Lab Bellevue and Tisch Hospitals
Anticoagulation in the cancer patient, and even more so with brain metastasis or primary brain tumors presents a classic Scylla versus Charybdis problem. Cancer patient are more thrombotic than non-cancer patients and also are more prone to bleeding. Despite the variation in patient specific risks, a universal approach has been adopted for VTE prophylaxis. ACCP recommends a formal strategy to reduce inpatient VTE which has been adopted by most hospitals. As this discussion highlights, there is also potential for harm. The field is now moving away from universal prophylaxis toward a risk adapted strategy for VTE prophylaxis in medical and surgical patients.
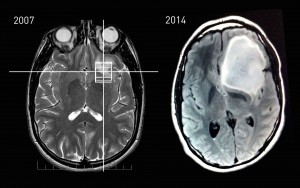
In this case, what if the brain MRI demonstrated evidence of microbleed (hemosiderin)? Should we alter our practice? These are the difficult questions we routinely face in real world practice.
Dr. Christopher Sonne is a 3rd year resident at NYU Langone Health
Peer Reviewed by David Green, MD, PhD, Clinical Assistant Professor, Division of Hematology/Oncology, Department of Medicine, NYU Langone Health
Image courtesy of Wikimedia Commons
References
- Lyman GH, Khorana AA, Falanga A, et al. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol 2007; 25:5490. https://www.ncbi.nlm.nih.gov/pubmed/17968019
- Weinstock, Matthew J., Erik J. Uhlmann, and Jeffrey I. Zwicker. “Intracranial hemorrhage in cancer patients treated with anticoagulation.” Thrombosis research 140 (2016): S60-S65. http://www.thrombosisresearch.com/article/S0049-3848(16)30100-1/fulltext
- Lee AY, et al. “Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer”. The New England Journal of Medicine. 2003. 349(2):146-53. http://www.nejm.org/doi/full/10.1056/NEJMoa025313#t=article
- Bergqvist, David. “Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep vein thrombosis in elective cancer surgery: a double-blind randomized multicentre trial with venographic assessment.” British Journal of Surgery 84.8 (1997): 1099-1103.
- Jo JT, Schif D, perry, JR. Thrombosis in brain tumors. Semin Thromb Hemost. 2014;40:325-31
- Yust-Katz S, Mandel JJ, Wu J, Yuan Y, Webre C, Pawar TA, et al. Venous thromboembolsim (VTE) and glioblastoma. J Neurooncol.2015;124:87-94
- Wen, Patrick Y., and J. S. Loeffler. “Management of brain metastases.” Oncology (Williston Park, NY) 13.7 (1999): 941-54. Accessed via http://www.cancernetwork.com/oncology-journal/management-brain-metastases. Jul 27 2016.
- Donato J, Campigotto F, Uhlmann EJ, et al. Intracranial hemorrhage in patients with brain metastases treated with therapeutic enoxaparin: a matched cohort study. Blood. 2015;126(4):494-499.
- Semrad TJ, O’Donnell R, Wun T, et al. Epidemiology of venous thromboembolism in 9489 patients with malignant glioma. J Neurosurg. 2007;106(4):601-608.
- Levin, J. M., et al. “Complications of therapy for venous thromboembolic disease in patients with brain tumors.” Neurology 43.6 (1993): 1111-1111.
- NCCN Clinical Practice Guidelines in Oncology. Venous Thromboembolic Disease. Accessed via http://www.nccn.org/professionals/physician_gls/PDF/vte.pdf. Jul 26 2016
- Olin JW, Young JR, Graor RA, et al: Treatment of deep vein thrombosis and pulmonary emboli in patients with primary and metastatic brain tumors: Anticoagulants or inferior vena cava filter? Arch Intern Med 147:2177-2179, 1987
- Perry, J. R., et al. “PRODIGE: a randomized placebo‐controlled trial of dalteparin low‐molecular‐weight heparin thromboprophylaxis in patients with newly diagnosed malignant glioma.” Journal of Thrombosis and Haemostasis8.9 (2010): 1959-1965.