Podcast: Play in new window | Download
Subscribe: RSS
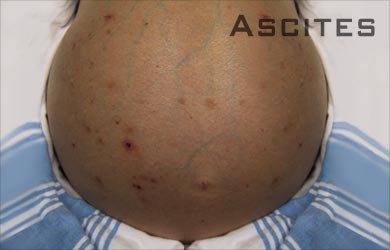
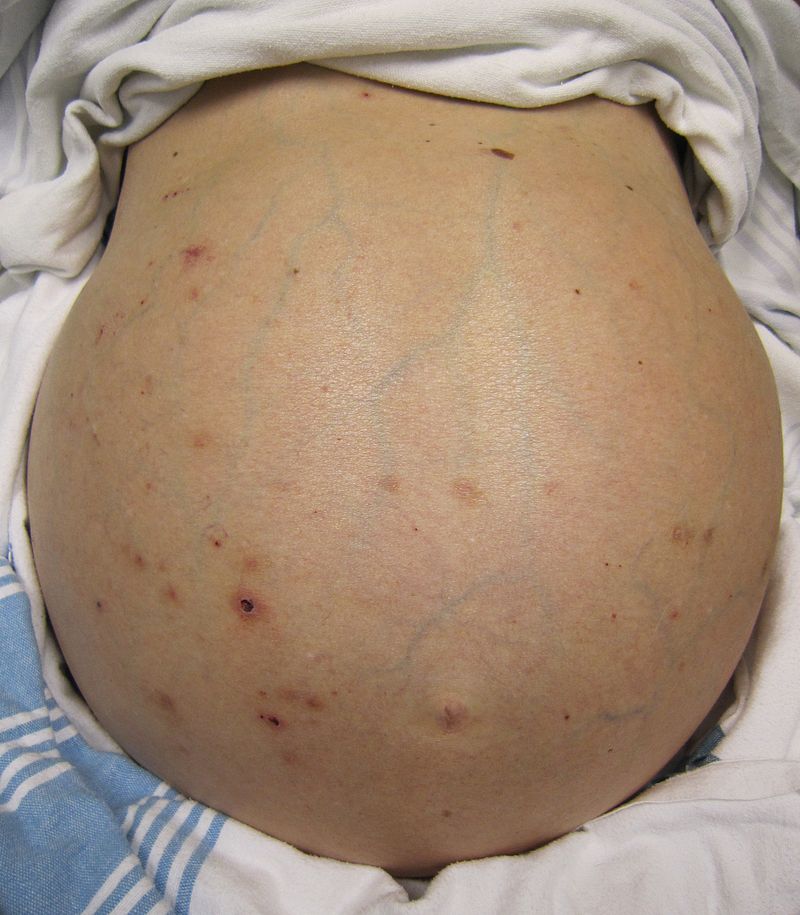 You have always been told to do a diagnostic paracentesis on admission in cirrhotics with ascites, but why? Can you just get away with clinical judgment to rule out SBP? Is faculty judgment any better? And if you’re going to do a paracentesis on admission, do you need to do it right away? Go deeper with Dr. Steven Liu and Dr. Janine Knudsen!
You have always been told to do a diagnostic paracentesis on admission in cirrhotics with ascites, but why? Can you just get away with clinical judgment to rule out SBP? Is faculty judgment any better? And if you’re going to do a paracentesis on admission, do you need to do it right away? Go deeper with Dr. Steven Liu and Dr. Janine Knudsen!
Time Stamps
- What do guidelines say about diagnostic paracentesis in cirrhotics with ascites? (1:51)
- Can we just use clinical judgment to decide if paracentesis is warranted? (3:13)
- Do attendings have better clinical judgment than residents to rule out SBP?
- Does timing of paracentesis on admission matter for mortality? (6:33)
Show notes:
- AASLD and European Association for the Study of the Liver guidelines recommend patients with cirrhosis and ascites admitted to the hospital should undergo a diagnostic abdominal paracentesis.
- In a prospective observational trial, physician clinical impression had a sensitivity of 76% and specificity of 34% for spontaneous bacterial peritonitis on admission
- Faculty tended to be more sensitive than residents, but not statistically significant.
- Don’t forget about asymptomatic SBP!
- Delayed paracentesis is associated with increased in-hospital mortality in patients with SBP comparing early paracentesis within 12 hours of admission vs. delayed between 12- 72 hours from admission.
- This corresponded to an increase in mortality of 3.3% for every hour delayed.
Many thanks to Dr. Renee Williams, Gastroenterologist at NYU, for peer reviewing this episode.
Subscribe to CORE IM on iTunes or Stitcher app! Follow us on Twitter @COREIMpodcast and Instagram @core.im.podcast. Please give any feedback to COREIMpodcast@gmail.com.
References:
1:57 – What does the AASLD recommend regarding abdominal paracentesis on arrival to the hospital? Runyon BA. “AASLD guidelines. Management of Adult Patients with Ascites Due to Cirrhosis: Update 2012” https://www.aasld.org/sites/default/files/guideline_documents/141020_Guideline_Ascites_4UFb_2015.pdf
3:17 – Chinnock B, et al. “Physician clinical impression does not rule out spontaneous bacterial peritonitis in patients undergoing emergency department paracentesis.” Ann Emerg Medˆ 2008 Sep;52(3)268-73. https://www.ncbi.nlm.nih.gov/pubmed/18433932
4:42 – Pinzello G, Simonetti RG, Craxi A, Di Piazza S, Spano C, Pagliaro L. “Spontaneous bacterial peritonitis: a prospective investigation in predominantly nonalcoholic cirrhotic patients.” Hepatology 1983 Jul-Aug;3(4):545-9 http://onlinelibrary.wiley.com.ezproxy.med.nyu.edu/doi/10.1002/hep.1840030411/abstract
5:43 – Angeli KL. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. https://www.easl.eu/medias/cpg/issue4/English-report.pdf
6:36 – Orman ES, Hayashi PH, Bataller R, Sidney Barritt IV A. “Paracentesis is associated with reduced mortality in patients hospitalized with cirrhosis and ascites.” Clin Gastroenterol Hepatol 2014 Mar;12(3):496-503 https://www.ncbi.nlm.nih.gov/pubmed/23978348
7:25 – Kim et al. “Delayed paracentesis is associated with increased in-hospital mortality in patients with spontaneous bacterial peritonitis.” Am J Gastroenterol 2014 Sep;109(9):1436-42 http://search.ebscohost.com.ezproxy.med.nyu.edu/login.aspx?direct=true&db=mnh&AN=25091061&site=ehost-live
Image courtesy of Wikimedia Commons