Vivian Hayashi MD, Robert Smith MD
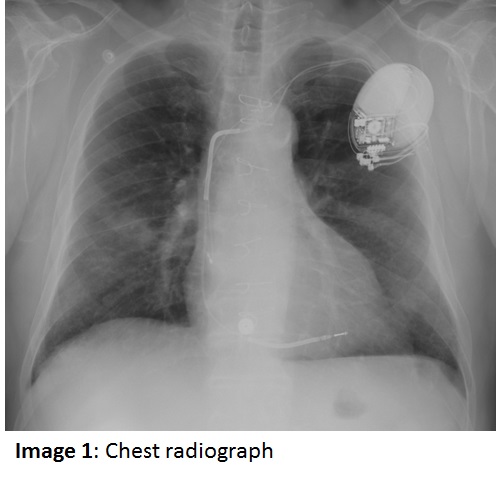
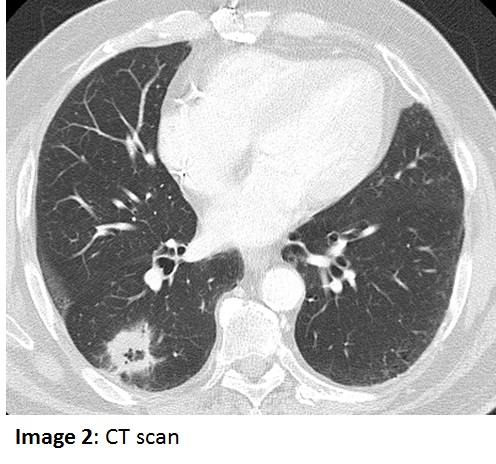
The patient is a 72 year old man who presented with an incidentally noted right mid-lung density on a chest radiograph. The patient was asymptomatic at the time and was begun on empiric treatment with moxifloxacin, then a course of amoxicillin-clavulanate for a presumed pneumonia (Image 1), without substantive improvement. A chest CT scan was subsequently obtained (Image 2). Further history was noteworthy for absence of hemoptysis, night sweats, fever, breathlessness, sputum production and weight loss. He did recall an episode of dark sputum production a few weeks earlier. The patient also denied coughing or choking while eating. The patient stopped drinking alcohol many years before but continued to smoke heavily. The past medical history includes coronary artery disease and CABG, and recent placement of a dual chamber pacemaker with an ICD for reduced LV ejection fraction. Physical exam revealed a pleasant man with normal vital signs, edentulous, clear chest to auscultation, without clubbing or palpable adenopathy. Lab values showed a WBC of 9.7k with a normal differential cell count, hemoglobin of 14.3 gm/dL, and normal serum electrolyte panel, including serum creatinine.