Peer Reviewed
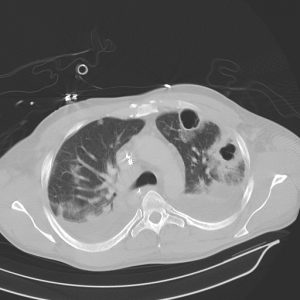
A 71-year-old Caucasian woman with hypertension presented with a 2-day history of productive cough and fever. She was living alone and had no history of any recent hospitalizations. On examination, she was alert and oriented but slightly tachypneic; her lungs were clear to auscultation bilaterally. Laboratory tests were significant for a white blood cell count of 18,000 mL with 89% neutrophils. The chest x-ray showed a right lower lobe infiltrate. She was admitted and started on antibiotics for treatment of community acquired pneumonia (CAP). She improved clinically, and after remaining afebrile for 48 hours, she was discharged on hospital day 3 on oral antibiotics. How long should the course of antibiotics be?
Why does this matter?
CAP is an acute infection of the lung parenchyma secondary to pathogens acquired within the community. According to the WHO in 2017, lower respiratory tract infections remain the deadliest communicable diseases, causing 3.2 million deaths in 2015.1 The annual incidence of CAP is approximately 5 to 11 cases per 1000 adults, resulting in more than 10 million visits to health care providers and 600,000 hospitalizations every year.2 In recent years, there has been a push to shorten antibiotic treatment for CAP in order to decrease bacterial resistance, reduce healthcare costs, and minimize adverse effects secondary to prolonged antibiotic use. In 2007, the Infectious Disease Society of America (IDSA) and American Thoracic Society (ATS) developed joint guidelines for the duration of antibiotic treatment. The guidelines recommend patients be treated for a minimum of 5 days, remain afebrile for 48 to 72 hours, and show no more than 1 sign of clinical instability.3 Despite these guidelines, duration of antibiotic treatment remains controversial and prolonged treatment is common. In 2016, Uranga et al. conducted a multicenter, noninferiority randomized clinical trial to validate the IDSA/ATS guidelines and to determine the optimal duration of antibiotic treatment for CAP.4
How was the study designed?
This multicenter, noninferiority randomized clinical trial was conducted in 4 teaching hospitals throughout Spain. Eligible patients were 18 years or older and hospitalized with a diagnosis of CAP. CAP was defined as a new pulmonary infiltrate on chest x-ray plus at least 1 clinical symptom of pneumonia, such as cough, fever, dyspnea, and/or chest pain. Patients were excluded if they were immunosuppressed, lived in a nursing home, had a recent hospitalization, were on a recent course of antibiotics, were recently admitted to the intensive care unit (ICU), had prior chest tubes, had complicated infections required prolonged antibiotics, or had any extrapulmonary infections. Patients were assessed for eligibility from day 0 to day 5 and then randomized on day 5 to either the intervention or control group. After 5 days of antibiotic therapy, treatment was discontinued in the intervention group if the patient had been afebrile for 48 hours and showed no more than 1 CAP-associated sign of clinical instability, which was defined as a systolic blood pressure less than 90 mm Hg, heart rate greater than 100/min, respiratory rate greater than 24/min, arterial oxygen saturation less than 90%, or PaO2 less than 60 mm Hg on room air. In the control group, duration of antibiotics was decided by the patients’ physicians. In both groups, antibiotics were chosen by physicians based on local guidelines.
The primary outcomes were clinical success rate at days 10 and 30, defined as resolution or improvement in clinical signs/symptoms of pneumonia, and CAP-related symptoms at day 10 using a validated 18-item CAP symptom questionnaire.5 Secondary outcomes were evaluated on day 30 to assess all-cause mortality and major complications such as CAP recurrence, readmissions, and adverse effects of antibiotics.
What were the results of the study?
There were 162 patients (mean age of 66.2 years) randomized to the intervention group, and 150 patients (mean age of 64.7 years) assigned to the control group. Baseline characteristics and demographics were similar in both groups. Additionally, both groups had similar vital signs at day 5 with mean pneumonia severity index scores of 81.8 and 83.7 respectively (P=0.55).
Clinical success rate at day 10 was 48.6% (71 of 150) in the control group and 56.3% (90 of 162) in the intervention group (P=0.18) in the intention-to-treat analysis with similar findings noted in the per-protocol analysis. At day 30, the clinical success rate improved to 88.6% (132 of 150) in the control group and 91.9% (147 of 162) in the intervention group (P=0.33) in the intention-to-treat analysis. The CAP symptom questionnaire scores were similar in both groups on day 5 (24.7 and 27.2 for control and intervention groups respectively; P=0.10) and day 10 (18.6 and 17.9 for control and intervention groups respectively; P=0.69).
Time receiving antibiotics was significantly longer in the control group than the intervention group (median, 10 days and 5 days, respectively, P< 0.001). Overall, there were no significant differences between the two groups in time until clinical improvement at day 30, radiographic resolution at day 30, adverse effects by day 30, in-hospital mortality, 30-day mortality, or in-hospital complications. Interestingly, 9 patients (6.6%) in the control group were readmitted to the hospital by day 30; only 2 patients (1.4%) were readmitted in the intervention group (P=0.02).
Are there any flaws to the study?
There are several limitations to this study, particularly regarding the generalizability of the results. The total sample size was small (312 patients) and included very few patients with severe pneumonia, defined as a pneumonia severity index class V, which makes it difficult to apply the findings to patients with more severe pneumonia. This challenge also applies to patients who received prior antibiotics, were immunosuppressed, needed a chest tube, or had a disease of an uncommon bacteriologic origin because they were excluded from the study. The study was conducted in 4 different hospitals throughout Spain, and although Streptococcal pneumoniae was the most common organism isolated from sputum cultures and Legionella pneumophila was second most common, the results may be difficult to extrapolate to other regions where certain pathogens may be more prevalent. Additionally, 80% of the patients received quinolones as the antibiotic regimen of choice, but there are many areas where beta-lactams and macrolides are the treatment of choice in clinical practice.
What is the bottom line?
This trial was the first multicenter randomized clinical trial performed to validate the use of IDSA/ATS guidelines for duration of antibiotic treatment in patients with CAP. In the setting of antibiotic overuse, increased microbial resistance, and elevated healthcare costs, this study offers support for shorter durations of antibiotic treatment for CAP based on clinical stability criteria.
Is this study a Game Changer?
We asked Dr. Melanie Maslow, Professor and Chief of Infectious Diseases at Manhattan Veteran Affairs (VA) Harbor Healthcare System, her opinion on how this trial translates into current clinical practice.
It has been a decade since the IDSA/ATS consensus guidelines on management of CAP were published. The guidelines recommend admitted patients not in the ICU be treated with a respiratory fluoroquinolone (FQ) or a beta-lactam plus a macrolide for a minimum of 5 days. Patients should be afebrile at 48 to 72 hours and show no more than 1 of the 7 CAP-associated signs of clinical instability before discontinuation of therapy.3 Despite the recommendations, few studies have been published to endorse the 5-day course. Dr. Ngai’s excellent review of this multicenter trial designed to validate duration of therapy in CAP provides us with new evidence supporting the 5-day duration in selected patients.4 The study excluded patients with immunocompromising conditions, with risk factors for and/or documented resistant pathogens, or in the ICU. Eighty percent of patients received a FQ. Patients in the intervention group, using IDSA/ATS criteria, received a median antibiotic course of 5 days compared with a median antibiotic duration of 10 days in the control, non-intervention, group. There were no statistically significant differences in clinical cure rates in the two groups. Dr. Ngai asks whether these results are a game changer for managing our patients.
The main take home message from this study is that despite the IDSA/ATS guidelines, most physicians in the control group prescribed antibiotic courses much longer than the 5-day minimum duration. In a small unofficial survey of internal medicine residents at the VA, only one had ever used a 5-day regimen and none were aware of the IDSA/ATS criteria for using a shorter course. At the VA, Bellevue, and Tisch Hospitals, ceftriaxone plus azithromycin is the most frequently used regimen for CAP. FQs are often reserved for patients with penicillin allergy due to concerns of potential serious adverse reactions, increasing resistance, and the link to nosocomial C. difficile infection with the BI/NAP1/027 strain.6 In my opinion, regardless of which IDSA/ATS approved regimen is used, this study is a potential game changer only in patients with CAP of mild to moderate severity, who are not immunocompromised, and with infection due to commonly encountered bacteria. Physicians should assess this subset of afebrile patients at 48 to 72 hours and use the clinical criteria to shorten duration of therapy to 5 days, if applicable. In addition to being equally effective as a longer course, as Dr. Ngai points out, a shorter course can decrease hospital stay, reduce emergence of resistance, and conserve resources.
Dr. Calvin Ngai is an internal medicine resident at NYU Langone Health
Peer reviewed by Melanie Maslow, MD, Professor and Chief of Infectious Diseases at Manhattan Veteran Affairs (VA) Harbor Healthcare System
Image courtesy of Wikimedia Commons
References
- WHO | The top 10 causes of death. WHO. 2017. http://www.who.int/mediacentre/factsheets/fs310/en/
- Mandell LA. Epidemiology and etiology of community-acquired pneumonia. Infectious disease clinics of North America. 2004;18(4):761-776, vii. https://www.ncbi.nlm.nih.gov/pubmed/15555823
- Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2007;44 Suppl 2:S27-72.
- Uranga A, Espana PP, Bilbao A, et al. Duration of Antibiotic Treatment in Community-Acquired Pneumonia: A Multicenter Randomized Clinical Trial. JAMA internal medicine. 2016;176(9):1257-1265. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2536189
- Lamping DL, Schroter S, Marquis P, Marrel A, Duprat-Lomon I, Sagnier PP. The community-acquired pneumonia symptom questionnaire: a new, patient-based outcome measure to evaluate symptoms in patients with community-acquired pneumonia. Chest. 2002;122(3):920-929.
- Vardakas KZ, Konstantelias AA, Loizidis G, Rafailidis PI, Falagas ME. Risk factors for development of Clostridium difficile infection due to BI/NAP1/027 strain: a meta-analysis. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2012;16(11):e768-773. https://www.ncbi.nlm.nih.gov/pubmed/22921930