Peer Reviewed
The Next Big Thing
For many physicians in training, navigating through the numerous anti-cancer agents and keeping pace with the latest treatments can be daunting. Major categories of systemic cancer treatments include chemotherapy (cytotoxic drugs that arrest the cell cycle), hormonal therapy (drugs that inhibit hormone production or bind to ‘starve’ cancers that thrive off of estrogen/testosterone), and targeted therapy (small molecules or monoclonal antibodies that bind to intra/extracellular targets to block tumor angiogenesis/growth factor signal transduction, or mark cells for destruction). The latest treatment class, immunotherapy, has taken center stage in our national health dialogue particularly with the recent New York Times feature, “Harnessing the Immune System to Fight Cancer.”[1] Former President Jimmy Carter’s public diagnosis of metastatic melanoma and remarkable remission has also heightened awareness. Given the increasing use of and public interest in immunotherapeutic regimens, medical providers should be aware of these therapies, the evidence behind them, and recognize their potential complications and toxicities.
The Mechanism of Immune Checkpoint Inhibitors
Though there are multiple treatment domains within “cancer immunotherapy,” a major source of excitement has been the discovery and the proven efficacy of immune checkpoint inhibitors – ipilimumab, nivolumab, pembrolizumab. These drugs operate on the basis that our own immune cells can recognize and eliminate both self-cells and malignant cells, but are usually inhibited from doing so by specific receptors and ligand complexes. These mechanisms normally serve to maintain self-tolerance and limit collateral tissue damage during immune responses, but are exploited by cancers to evade immune effector cells.[2]
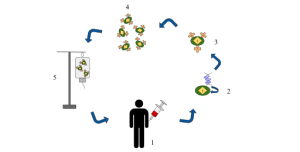
Briefly, immune checkpoints essentially occur during the 1) priming/activation and 2) effector phases for T-cells. In priming, an antigen/major histocompatibility complex is presented to a T-cell receptor, and is accompanied by either a co-stimulatory or co-inhibitory receptor signal that results in subsequent activation or inhibition of that T-cell.[3] Cytotoxic lymphocyte-associated protein 4 (CTLA-4) is a co-inhibitory receptor/protein complex that is overexpressed in many cancers; its binding results in inhibition of naïve and memory T-cell function, leading to development of cancer antigen tolerance.[3] The monoclonal antibody ipilimumab targets CTLA-4, blocking the inhibitory signal and, in turn, promoting T-cell priming/activation. Once briefed and sent on their seek-and-destroy mission, cytotoxic T-lymphocytes (CTLs) face co-inhibitory signaling during their effector phase, from the binding of programmed cell death protein (PD-1) receptor and its ligand PD-1L. Cancer cells limit host immune response by upregulating PD-1L in the tumor microenvironment, and their binding to PD-1 leads to T-cell apoptosis, anergy, and downregulated cytokine production.[3,4] Nivolumab and pembrolizumab are monoclonal antibodies that block PD-1L from binding with PD-1, thwarting inhibition of CTLs, thus allowing them carry out their mission of destroying malignant cells.
Where’s the Proof?
In 2010, anti-CTLA-4 agent ipilimumab was the first treatment to show a significantly improved survival rate in patients with metastatic melanoma that progressed following initial therapy.[5] After a few years, ipilimumab became first line therapy in advanced melanoma.[6] For patients whose disease progressed despite treatment with ipiliumumab, PD-1 blockers such as nivolumab were later introduced, and showed greater clinical response with fewer toxic effects than alternative chemotherapy regimens.[7] PD-1 checkpoint inhibitors then became the preferred first-line agent when pembrolizumab was shown to have prolonged progression-free survival (PFS), overall survival (OS), and better tolerance than ipilimumab in treatment-naïve, advanced melanoma.[8] Similarly, nivolumab alone or nivolumab combined with ipilimumab, resulted in significantly longer PFS than ipilimumab alone.[9] It should be noted, in patients with PD-L1-negative tumors, the combination of PD-1 and CTLA-4 blockade was more effective than either agent alone.[8]
PD-1 blockers also proved to be a promising second-line therapy for advanced squamous cell non-small cell lung cancer (NSCLC) patients who had failed first-line platinum doublet-based chemotherapy, based on data showing that nivolumab had superior OS compared to then-standard second-line chemotherapy, docetaxel.[10] Even more recently, patients with untreated advanced NSCLC, with at least 50% of tumor cells expressing PD-L1 treated with pembrolizumab, had better PFS, OS, and tolerance even compared to first-line platinum-based chemotherapy.[11] PD-1 blockers are also a promising second-line agent in advanced renal cell carcinoma,[12] and other phase III studies in numerous other malignancies are currently on-going.
Identifying and Managing Adverse Effects
The augmented immune response spurred by checkpoint inhibitors results in enhanced anti-tumor activity but unfortunately also causes unique types of collateral damage called immune-related adverse events (IRAEs) as a consequence of impaired self-tolerance from loss of T-cell inhibition. IRAEs tend to follow a predictable pattern, with rashes and GI toxicity seen early and liver toxicity or endocrinopathies seen later in the treatment course. [13] Certain IRAEs appear to be specific to certain cancers treated with immune check point inhibitors, with pneumonitis being more prevalent in lung cancer patients and higher rates of vitiligo and colitis observed in melanoma patients.[14] In general, the anti-PD-1 antibodies nivolumab and pembrolizumab are are more tolerable (10-15% rate of grade 3 [severe] and 4 [life-threatening] adverse events (AEs)) compared to ipilimumab (20–30% rate of grade 3-4 AEs) or combination PD-1 + CTLA-4 blockade therapy (55% rate of AEs).[14] Immune modulators (IMMs) are employed for high grade IRAEs and most patients achieve control with steroids or infliximab for steroid-refractory toxicity.[3] Fortunately, it has been shown that treating IRAEs with steroids/IMMs has yet to show any detrimental effect on the efficacy of immune check point therapy in terms of OS and PFS.[15]
Closing Thoughts
As immunotherapies, like checkpoint inhibitors, become staples of cancer treatment across organ sites and cell types, it will become increasingly important for physicians to develop a sophisticated understanding of the mechanisms, research, and adverse effects of these therapies to better care for their patients. Furthermore, physicians in training will be a key source of knowledge regarding these paradigm-shifting treatments as continue to gain recognition and bring a newfound sense of optimism to the fight against cancer.
Commentary by Daniel Becker, MD Section Chief Hematology/Oncology VA New York Harbor Healtcare System
Immune checkpoint inhibitors offer new hope to tens of thousands of patients with cancer, and new insight into the critical role of the immune system in cancer surveillance and control. In addition to the aforementioned approvals in melanoma and non-small cell lung cancer, checkpoint inhibitors now have a proven role in urothelial carcinoma, head and neck cancers, Hodgkins Lymphoma, renal cell carcinoma, and, as of May 23, 2017, microsatellite-high (MSI-H), or DNA mismatch repair deficient cancers of any type. This last approval is the first site agnostic FDA approval, i.e. unrelated to the cancer site of origin. Microsatellites are non-coding regions of DNA and a likely spot for replication errors in patients whose DNA repair apparatus is ineffective. Theoretically the increased mutational burden in patients who are MSI-H increases the array of neoantigens presented to the immune system, enabling improved cancer surveillance. Colon cancer, previously considered a poorly immunogenic cancer, includes a subset of approximately 15% of patients with MSI-H cancers, including the Lynch Syndrome cancers. The approval of pembrolizumab for patients with MSI-H cancers was based on 149 heavily pretreated patients with various tumor types who showed a response rate of 40%, with 78% of the responses lasting more than 6 months. Although oncologists are often skeptical about headlines over-selling the latest cancer developments, the checkpoint inhibitors are truly revolutionary. We enthusastically await further development of the checkpoint inhibitors, and further improvements in the lives of cancer patients.
Dr. Thatcher Heumann is an internal medicine resident at NYU Langone Health
Peer reviewed by Daniel Becker, MD, Medical Oncology, NYU Langone Health
Image courtesy of Wikimedia Commons
References
1. Grady D. Harnessing the Immune System to Fight Cancer. The New York Times 2016. http://www.nytimes.com/2016/07/31/health/harnessing-the-immune-system-to-fight-cancer.html?_r=0. Accessed 15 Nov 2016.
2. Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell. 2015;27(4):450-461.
3. La-Beck NM, Jean GW, Huynh C, Alzghari SK, Lowe DB. Immune Checkpoint Inhibitors: New Insights and Current Place in Cancer Therapy. Pharmacotherapy. 2015;35(10):963-976. https://www.ncbi.nlm.nih.gov/pubmed/26497482
4. Boussiotis VA. Molecular and Biochemical Aspects of the PD-1 Checkpoint Pathway. N Engl J Med. 2016;375(18):1767-1778. https://www.ncbi.nlm.nih.gov/pubmed/27806234
5. Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711-723. https://www.ncbi.nlm.nih.gov/pubmed/20525992
6. Franklin C, Livingstone E, Roesch A, Schilling B, Schadendorf D. Immunotherapy in melanoma: Recent advances and future directions. Eur J Surg Oncol. 2016.
7. Weber JS, D’Angelo SP, Minor D, Hodi FS, Gutzmer R, Neyns B, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16(4):375-384.
8. Robert C, Schachter J, Long GV, Arance A, Grob JJ, Mortier L, et al. Pembrolizumab versus Ipilimumab in Advanced Melanoma. N Engl J Med. 2015;372(26):2521-2532.
9. Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Cowey CL, Lao CD, et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. N Engl J Med. 2015;373(1):23-34.
10. Brahmer J, Reckamp KL, Baas P, Crino L, Eberhardt WE, Poddubskaya E, et al. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N Engl J Med. 2015;373(2):123-135.
11. Reck M, Rodriguez-Abreu D, Robinson AG, Hui R, Csoszi T, Fulop A, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med. 2016.
12. Motzer RJ, Escudier B, McDermott DF, George S, Hammers HJ, Srinivas S, et al. Nivolumab versus Everolimus in Advanced Renal-Cell Carcinoma. N Engl J Med. 2015;373(19):1803-1813.
13. Weber JS, Yang JC, Atkins MB, Disis ML. Toxicities of Immunotherapy for the Practitioner. J Clin Oncol. 2015;33(18):2092-2099.
14. Spain L, Diem S, Larkin J. Management of toxicities of immune checkpoint inhibitors. Cancer Treat Rev. 2016;44:51-60.
15. Horvat TZ, Adel NG, Dang TO, Momtaz P, Postow MA, Callahan MK, et al. Immune-Related Adverse Events, Need for Systemic Immunosuppression, and Effects on Survival and Time to Treatment Failure in Patients With Melanoma Treated With Ipilimumab at Memorial Sloan Kettering Cancer Center. J Clin Oncol. 2015;33(28):3193-3198.