Peer Reviewed
With medicine advancing at such a rapid pace, it is crucial for physicians to keep up with the medical literature. This can quickly become an overwhelming endeavor given the sheer quantity and breadth of literature released on a daily basis. Primecuts helps you stay current by taking a shallow dive into recently released articles that should be on your radar. Our goal is for you to slow down and take a few small sips from the medical literature firehose.
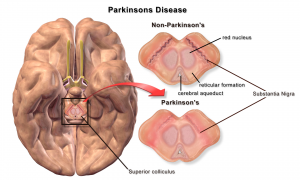
The vermiform appendix impacts the risk of developing Parkinson’s disease [1]
In this unique study, researchers investigated the role of the vermiform appendix in Parkinson’s disease (PD). The association stems from GI dysfunction being a common early Parkinsonian symptom, as well as α-synuclein aggregates having been discovered within enteric neurons of the GI tract, before the onset of motor symptoms. This epidemiological study drew from two data sets, for more than 1.6 million patients total. Among those who had an appendectomy, the incidence of PD (1.60 per 100,000 person years, CI 95%, 1.46-1.75) was lower than among those who did not undergo appendectomy (1.98, 1.87-2.10). This represented a 19.3% decrease in risk (95% CI, 10.4-27.2%, P <0.0001). The prevalence of PD in patients who had appendectomies was also lower, by 16.9% (CI 95%, 9.3-24.4%, P <0.0001). Furthermore, the study looked at age of onset of PD among patients with or without appendectomy. The average age of PD diagnosis was 1.6 years later in individuals who underwent appendectomy 20 years or more prior (95% CI, -0.09-3.34, P <0.03). This is certainly a fascinating connection to draw, but the concept of prophylactic appendectomy seems unlikely to catch on. The association between the appendix and PD may be more valuable toward our understanding of the disease than actual clinical practice. As James Beck, PhD, Chief Scientific Officer of the Parkinson’s Foundation, put it: “It connects the epidemiology…with the basic science.” [1]
Traditionally, COPD treatment begins with monotherapy – using a long-acting muscarinic antagonist, long-acting beta agonist, or inhaled corticosteroid – and is then escalated to dual therapy or triple therapy as needed. This study sought to compare the rate of COPD exacerbations (moderate to severe) under those three approaches through a meta-analysis of 21 randomized control trials. Compared to LAMA monotherapy, triple therapy reduced the rate of moderate or severe exacerbations (rate ratio 0.71, 95% CI 0.60-0.85) as well as the number of patients having a moderate or severe exacerbation (risk ratio 0.74, 95% CI 0.56-0.97). Triple therapy also increased time to first moderate or severe exacerbation (hazard ratio 0.69, 95% CI 0.54-0.88). There were similar findings when comparing triple therapy to LAMA-LABA and LABA-ICS dual therapy. All-cause mortality, however, was not significantly decreased by triple therapy. Additionally, triple therapy showed a higher incidence of pneumonia. Overall, triple therapy appears to decrease exacerbation rates, but has no real effect on patient survival, and may increase the risk of pneumonia. As such, clinicians might still consider limiting triple therapy to patients with more severe symptoms that are resistant to dual therapy alone.
In 2014, the US CDC Advisory Committee on Immunization Practices updated their pneumococcal vaccination recommendations to include PCV13 use for all adults over the age of 65. This study sought to evaluate the effectiveness of PCV13 in protecting against vaccine type (VT) CAP using an observational test-negative design. Researchers used data from 2034 elderly patients hospitalized for CAP. Vaccine efficacy (VE) of PCV13, unadjusted, was 72.8% (95% CI, 12.8%-91.5%). The investigators also looked at the proportion of hospitalized PCV13 serotype CAP patients by vaccination status. CAP patients who had received the PCV13 were less likely to have detectable PCV13 serotypes (3/288, 1%) than those who did not receive the PCV13 (65/1746, 3.7%), with a P value of 0.02. The VE in this study, 72.8%, was significantly higher than the VE of 46% that was seen in the original CAPiTA study that led to the 2014 CDC recommendation. Of note, this study was observational in design, and not an RCT like CAPiTA. Reserachers relied on insurance company information to verify vaccination status so patients may have been incorrectly labeled as unvaccinated. Finally, the number of PCV13 serotype cases (68) was rather small compared to controls (1966). Nonetheless, this study demonstrates the ability of PCV13 vaccination to cut down the hospitalization rate for CAP, the duration of hospital stay, and the number of deaths from CAP. Given the low risk of vaccination, and the potential public health benefit, PCV13 vaccination continues to seem like a no-brainer.
sST2 Predicts Outcome in Chronic Heart Failure Beyond NT−proBNP and High-Sensitivity Troponin T [5]
sST2 is a biomarker associated with activation of inflammatory and pro-fibrotic pathways. It has a narrow range of variation, and compared to NT-proBNP is less influenced by age, sex, BMI, and other disease processes. This study, therefore, set out to assess sST2 as an independent prognostic marker in CHF, beyond NT-proBNP and hs-TnT. Researchers conducted a meta-analysis of data from 4,268 patients. The population was divided based on median values of the 3 biomarkers. Compared to those with biomarkers below the median, patients with sST2 at or above the median had an increased risk of all-cause death (100%), cardiovascular death (50%), and CHF hospitalization (10%). Researchers developed a prognostic model including a multitude of factors, and with each doubling of sST2, the risk of all-cause death increased by 26% (hazard ratio 1.58, 95% CI 1.48-1.68, P <0.001), the risk of cardiovascular death increased by 25% (hazard ratio 1.51, 95% CI 1.40-1.62, P <0.001), and the risk of CHF hospitalization increased by 30% (hazard ratio 1.58, 95% CI 1.47-1.69, P <0.001). sST2 measurement provided prognostication for all 3 endpoints, independent of NT-proBNP and hs-TnT, and was unaffected by the presence of comorbidities and systemic inflammation. It appears that sST2 could be added to standard heart failure lab testing and help guide clinical decision-making. Barriers to implementation would be cost and availability of such an assay. It seems unlikely that we will see sST2 assays available in hospitals across the country anytime soon. Given the data backing sST2 as a standalone prognostic marker, however, it seems likely that this biomarker will now be part of the discussion around CHF stratification and treatment.
Minicuts
Changes in Prevalence of Health Care–Associated Infections in U.S. Hospitals [6]
Health care-associated infections have gained more attention recently, so four years after a point-prevalence survey revealed 4% of US hospitalized patients acquired such infections, the same survey was repeated to see if any progress had been made. Researchers found a significant reduction in infections, down to 3.2%, but work remains to be done in curbing health care-associated c. difficile infection and pneumonia.
One-Year Outcomes after PCI Strategies in Cardiogenic Shock [7]
This study looked at outcomes one year after PCI was performed for patients in cardiogenic shock, with the primary difference being PCI of only the culprit lesion versus immediate multivessel PCI. There was no significant difference in mortality at one year between the two groups, but those who had culprit-vessel PCI alone had higher rates of hospitalization for heart failure and for repeat revascularization.
Reduced Salt Intake for Heart Failure: A Systematic Review [8]
This systematic review of nine studies sought to evaluate whether reduced dietary salt intake led to clinical improvement of heart failure. Data was mostly insufficient to suggest reduced salt intake affected outcomes such as mortality or hospitalization, despite this being a very common recommendation.
Platelet Microparticles Mediate Glomerular Endothelial Injury in Early Diabetic Nephropathy [9]
Platelet microparticles are extracellular vesicles released by activated platelets, and they are suspected to contribute to vascular dysfunction. As such, these microparticles may play a key role in the development of early diabetic nephropathy. In this study, diabetic rats demonstrated markedly increased levels of platelet microparticles, and a microparticle-derived ligand, CXCL7, was shown to have a key role in glomerular endothelial injury. Targeting this ligand may be beneficial for treating early diabetic nephropathy.
Dr. Nathaniel Siev, MD is a first year internal medicine resident at NYU Langone Health
Peer reviewed by Christian Torres MD, Associate Editor, Clinical Correlations
Image courtesy of Wikimedia Commons
Reference:
- Killinger BA, et al. The vermiform appendix impacts the risk of developing Parkinson’s disease. Science Translational Medicine. 2018;10(465):1-15. doi:10.1126/scitranslmed.aar5280
- https://www.beckershospitalreview.com/quality/appendectomy-linked-to-20-lower-parkinson-s-risk-for-some-patients-study-finds.html
- Zheng Yayuan, et al. Triple therapy in the management of chronic obstructive pulmonary disease: systematic review and meta-analysis BMJ 2018; 363 :k4388 https://www.bmj.com/content/363/bmj.k4388
- John M McLaughlin, et al; Effectiveness of 13-Valent Pneumococcal Conjugate Vaccine Against Hospitalization for Community-Acquired Pneumonia in Older US Adults: A Test-Negative Design, Clinical Infectious Diseases, Volume 67, Issue 10, 30 October 2018, Pages 1498–1506, https://doi.org/10.1093/cid/ciy312
- Michele Emdin, et al. sST2 Predicts Outcome in Chronic Heart Failure Beyond NT−proBNP and High-Sensitivity Troponin T Journal of the American College of Cardiology Nov 2018, 72 (19) 2309-2320; DOI: 10.1016/j.jacc.2018.08.2165
- Shelley S. Magill, et al. Changes in Prevalence of Health Care–Associated Infections in U.S. Hospitals N Engl J Med 2018; 379:1732-1744 DOI: 10.1056/NEJMoa1801550 https://www.nejm.org/doi/full/10.1056/NEJMoa1801550
- Holger Thiele, et al. One-Year Outcomes after PCI Strategies in Cardiogenic Shock N Engl J Med 2018; 379:1699-1710 DOI: 10.1056/NEJMoa1808788 https://www.nejm.org/doi/full/10.1056/NEJMoa1808788
- Mahtani KR, et al. Reduced Salt Intake for Heart Failure A Systematic Review. JAMA Intern Med. doi:10.1001/jamainternmed.2018.4673 https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2712563
- Yang Zhang, et al. Platelet Microparticles Mediate Glomerular Endothelial Injury in Early Diabetic Nephropathy JASN Nov 2018, 29 (11) 2671-2695; DOI: 10.1681/ASN.2018040368 https://jasn.asnjournals.org/content/early/2018/10/18/ASN.2018040368/tab-article-info?versioned=true