Podcast: Play in new window | Download
Subscribe: RSS
By Vishal Shah MD, Milna Rufin MD, Marty Fried MD, Shreya P. Trivedi MD || Illustration by Amy Ou MD || Audio Editing by Harit Shah. Quiz yourself on the 5 Pearls we will be covering:
- What is Barrett’s esophagus? (4:12)
- Who do we screen for Barrett’s, and why? (8:41)
- How do we screen for Barrett’s and counsel? (13:50)
- How do we treat and monitor Barrett’s esophagus? (18:21)
- Take Aways (21:45)
- Throwback to trending troponins (23:05)
Thank you to peer-reviewers Dr. Nicholas Shaheen, Dr. David Katzka, and Dr. Joe Kingsbery.
Subscribe to CORE IM on any podcast app! Follow us on Facebook @Core IM || Twitter @COREIMpodcast || Instagram @core.im.podcast. Please give any feedback at COREIMpodcast@gmail.com.
Show Notes
Pearl 1: What is Barrett’s esophagus?
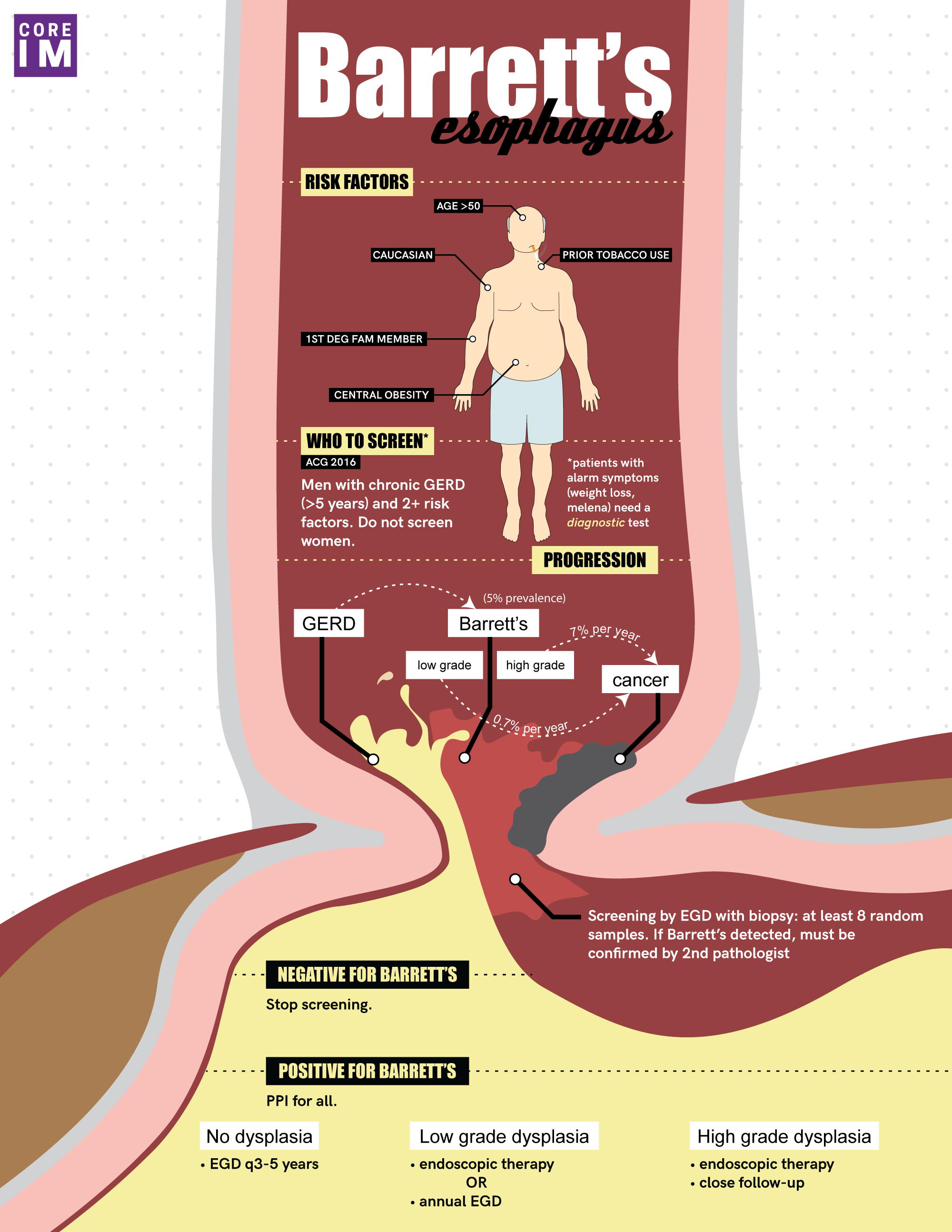
- Barrett’s esophagus is metaplasia of the normal squamous epithelium of the esophagus to columnar epithelium.
- Estimated prevalence of Barrett’s in the general population is 5%, and the majority have do not have dysplasia, but if there is high grade dysplasia, there is a 7% annual risk of developing adenocarcinoma, which is what we ultimately want to prevent.
Pearl 2: Who do we screen for Barrett’s, and why?
- According to the American College of Gastroenterology (ACG), we should screen men who have chronic GERD and have at least two risk factors: Caucasian race, age over 50 years, any smoking history, central obesity, or a 1⁰ relative with barrett’s or esophageal adenocarcinoma.
Pearl 3: How do we screen for Barrett’s and counsel if they do have Barrett’s?
- Screening is done with an upper endoscopy (EGD) with 8 biopsies and is specially reviewed by expert pathologists.
- The majority of patients with Barrett’s will have the nondysplastic type. Per Dr. Shaheen, it should be phrased to the patient as, “This is a chronic disease like any other chronic disease, diabetes, hypertension, etc. We check certain parameters to make sure that you’re not having your disease worsen, you should think about this. The overall risk of progression is quite low.”
Pearl 4: How do we treat and monitor Barrett’s esophagus?
- Patients with Barrett’s esophagus should be on a once daily PPI because of its chemoprotective nature, even in the absence of GERD symptoms.
- Patients with nondysplastic Barrett’s should be reassured that there is low rate of progression, and should have repeat EGD every 3-5 years for surveillance.
- If there is low grade dysplasia, the patient can choice between surveillance with more frequent EGDs or radiofrequency ablation.
- If there is high grade dysplasia, first-line treatment is radiofrequency ablation followed by routine surveillance.
Pearl 5: Throwback to trending troponins
- The delta, or change in between the two values of troponin, can help guide suspicion for ACS in less clear cases.
References
- Bani-Hani KE, Bani-Hani BK. Columnar-lined esophagus: time to drop the eponym of “Barrett” Historical review. J Gastroenterol Hepatol 2008;23:707–15. https://www.ncbi.nlm.nih.gov/pubmed/18410605
- Coleman HG, Xie SH, Lagergren J. The Epidemiology of Esophageal Adenocarcinoma. Gastroenterology. 2018;154:390–405. https://www.ncbi.nlm.nih.gov/pubmed/28780073
- Desai TK, Krishnan K, Samala N et al. The incidence of oesophageal adenocarcinoma in non-dysplastic Barrett’s oesophagus: a meta-analysis. Gut 2012;61:970–976. https://gut.bmj.com/content/61/7/970.long
- Feldman M, Friedman L, Brandt L. (2016). Sleisenger and Fordtran’s gastrointestinal and liver disease. 10th ed. Philadelphia: Moises Ilan Nevah, pp.755-762.
- Fletcher J, Wirz A, Henry E, et al. Studies of acid exposure immediately above the gastro-oesophageal junction: Evidence of short segment reflux. Gut 2004; 53:168-73. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1774939/
- Hayeck T.J., Kong C.Y., Spechler S.J., Gazelle G.S., Hur C. The prevalence of Barrett’s esophagus in the US: estimates from a simulation model confirmed by SEER data. Dis Esophagus. 2010;23:451–457. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2896446/
- Rastogi A, Puli S, El-Serag HB et al. Incidence of esophageal adenocarcinoma in patients with Barrett’s esophagus and high-grade dysplasia: a meta-analysis. Gastrointest Endosc 2008;67:394–398. https://www.ncbi.nlm.nih.gov/pubmed/18045592
- Shaheen NJ, Falk GW, Iyer PG, Gerson LB American College of Gastroenterology. ACG Clinical Guideline:Diagnosis and management of Barrett’s esophagus. Am J Gastroenterol. 2016;111:30–50. https://gi.org/guideline/diagnosis-and-management-of-barretts-esophagus/
- Shaheen NJ, Weinberg DS, Denberg TD, Chou R, Qaseem A, Shekelle P, et al. Upper Endoscopy for Gastroesophageal Reflux Disease: Best Practice Advice From the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med. 2012;157:808–816. https://annals.org/aim/fullarticle/1470281/upper-endoscopy-gastroesophageal-reflux-disease-best-practice-advice-from-clinical
- Sikkema M, de Jonge PJ, Steyerberg EW, Kuipers EJ. Risk of esophageal adenocarcinoma and mortality in patients with Barrett’s esophagus: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2010;8:235–244. https://www.ncbi.nlm.nih.gov/pubmed/19850156
- Singh S, Manickam P, Amin AV et al. Incidence of esophageal adenocarcinoma in Barrett’s esophagus with low-grade dysplasia: a systematic review and meta-analysis. Gastrointest Endosc 2014;79:897–909. https://www.ncbi.nlm.nih.gov/pubmed/24556051
- Spechler SJ, Souza RF. Barrett’s esophagus. N Engl J Med 2014;371:836-45. https://www.ncbi.nlm.nih.gov/pubmed/25162890