Peer Reviewed
With medicine advancing at such a rapid pace, it is crucial for physicians to keep up with the medical literature. This can quickly become an overwhelming endeavor given the sheer quantity and breadth of literature released on a daily basis. Primecuts helps you stay current by taking a shallow dive into recently released articles that should be on your radar. Our goal is for you to slow down and take a few small sips from the medical literature firehose.
Diabetes is one of the most common conditions seen in both the hospital and clinic. It has many complications, including cardiovascular ones, and also raises cardiovascular risk. With the surge in new diabetes medications, the comparison between new and old treatments becomes increasingly relevant. Furthermore, the safety and efficacy of sulfonylureas has long been a topic of debate. Concerns about weight gain, hypoglycemia (seen in this trial), and cardiotoxicity are some reasons many avoid sulfonylureas. However, their low cost and the medical and patient community’s familiarity leads to continued use. [2] This trial investigated the safety and efficacy of a DPP4 inhibitors against a sulfonylurea.
The CAROLINA trial was a randomized, double-blind, prospective, worldwide, multicenter trial comparing linagliptin vs. glimepiride for reducing cardiovascular risk. Primary outcome was time to either cardiovascular death, nonfatal myocardial infarct, or nonfatal stroke. It makes sense this study was designed to test for non-inferiority given many practitioner’s reservations about the side effects of sulfonylureas.
Six thousand-forty-two patients participated in this study (40% women). Median follow up time was 6.3 years. Around 40% of participants already had diagnosed macrovascular disease. Three thousand twenty-eight patients were randomized to receive linagliptin, and 3014 were randomized to receive glimepiride. Patients receiving glimepiride started receiving 1mg daily and were titrated to 4 mg as tolerated. There were no major differences between treatment groups at the start of the study. They sought to establish non inferiority through the upper limit of 95.5% two sided confidence interval for a hazard ratio of 1.3.
Both groups were similar, as in non-inferior to one another, in regards to primary end point of combined rate of cardiovascular death, non-fatal myocardial infarct, or non-fatal stroke. Both groups had 2.1 of these events per 100 patient years. Both groups had similar rates of cardiovascular death. In regards to the secondary endpoint, more patients on linagliptin were on treatment without major weight gain, and had A1C less than or equal to 7% at final study visit, with a hazard ratio of 1.29 (1.12-1.48 95% CI). Overall though, there were no major inter group differences for adjusted mean change in A1C. There were no differences between groups in terms of all-cause mortality. The study authors note “modest weight gain” seen early in the study and then maintained, in the glimepiride group. This is consistent with what is known about sulfonylureas.
Adverse events occurred to 93.4% of participants in the linagliptin group, and 94.9 of participants in the glimepiride group. Both groups had similar rates of discontinuation due to side effects. Slightly more patients on glimepiride had hospitalizations. The patients in the glimepiride group had significantly more hypoglycemia events, consistent with a known side effect.
This study helps to validate practitioners who are averse to sulfonylureas, but uncertain about the alternatives. It elucidates the similar efficacy of sulfonylureas and DPP4 inhibitors. It also helps support practitioners in their care for diabetic patients, and may help them feel more comfortable switching from one medication class to another.
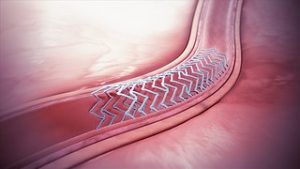
Five-Year Outcomes After PCI or CABG for Left Main Coronary Disease [3]
The debate between PCI and CABG for patients with CAD is a hotly and long debated topic in academic medicine. This study adds new insights into this rich body of literature.
This randomized, prospective, multicenter trial analyzed 1,905 patients and followed their course for five years after intervention. They recruited patients with left main coronary disease, determined to have low or intermediate anatomical complexity. They randomized 948 patients to PCI, and 957 to CABG. The primary outcome was the composite of death from any cause, stroke, or myocardial infarct at three years. Long-term secondary measures included these data points but at five years. They previously published data in 2016 on their three-year outcomes, and this paper is an update at five years.
In both groups, approximately 20% of patients died or had a stroke or MI at five years, with no significant difference. There was a slightly higher rate of death from any cause at five years in the group of patients randomized to PCI, with an odds ratio of 1.38 (95% CI, 1.03-1.85). Patients who underwent PCI had higher rates of ischemia-driven revascularization at five years, with an OR of 1.84 (,95% CI, 1.39-2.44). As expected, regarding short-term outcomes, patients who underwent CABG had higher combined rates of death, stroke, or MI within 30 days of the index procedure. However, there were not higher rates of death in the CABG group.
Overall, this study did not find a significant difference between CABG and PCI for patients with left main CAD in terms of major outcomes at five years. This study adds to the current literature on this debate, including patients receiving newer-generation, everolimus drug-eluting stents. The SYNTAX study came out in 2009 and demonstrated in patients with three-vessel or left main CAD, CABG was superior in terms of one-year outcomes. However, they performed PCI with paclitaxel-eluting stents.
A weakness of this study is the criteria of anatomical complexity. It would be interesting to see how patients with more complex anatomy would fare in a similar study, although in clinical practice it is likely they would undergo CABG. Another weakness is that the study was originally designed and powered for a primary endpoint of outcomes at three years. This update, at five years, therefore may be underpowered.
This is a question I think about frequently, and something I think many physicians, especially ones responsible for drawing blood cultures and ordering antibiotics, worry about. This is especially relevant as we learn more and more and are reminded more and more about the consequences of untreated sepsis.
This prospective study was conducted at seven emergency rooms throughout North America between 2013 and 2018. Adults with signs of severe sepsis, including lactate of greater than 4, or systolic blood pressure below 90, were included in the study. There were 3,164 patients screened, but only 325 participants who were included in the study. 61 patients were further excluded from the strict per-protocol analysis. Patients had two sets of blood cultures drawn before antibiotics, and two sets drawn within two hours after antibiotics.
Mean patient age was 65.6 years old. Median time to repeating cultures after antibiotics was 70 minutes. The respiratory tract was the most common source of infection in the entire analyzed study population.
Pre-treatment blood cultures were positive in 102 patients. This is 31.4% of the study population. Post-treatment cultures were positive in 63 patients. Ten patients had blood cultures positive for a contaminant before treatment and were excluded. Six had cultures with contaminants after treatment and were excluded from analysis. The absolute difference in the proportion of bacteremic blood cultures before and after antibiotics was 12%.
This study confirms the fact that delaying cultures until after antibiotics reduces sensitivity and yield. However, researchers also found that patients with positive pre-treatment blood cultures were more likely to have subsequent respiratory failure. Therefore, again, it is ideal to get antibiotics first. This study also confirms that starting antibiotics quickly in patients with presumed bacteremia is the highest priority.
Study authors also mention there was a group of participants who had their second set of blood cultures drawn too late, outside of the window in the protocol. They were excluded from final analysis, but had results similar to the rest of the study. This also shows the challenges of drawing cultures quickly in a busy ER or other busy service.
A weakness of this study is the relatively small sample size and strict protocol. The authors also noted how some institutions in the study required slight alterations from the protocol in terms of number and timing of blood cultures. They also amended the protocol to allow for blood cultures being drawn up to four hours after antibiotics. These weaknesses could change the data and interpretation of it slightly. However, they do not seem to detract from the overall results and summary message of this study. A possible next step would be to study which types of bacteria are more likely to not be seen after administering antibiotics.
Minicuts
Update on the pathogenesis of COPD [5]
For many years, the classic understanding of COPD was destruction of alveoli, with chronic bronchitis and increased mucus production, combined with lung aging at baseline. However, recent studies have shown us the complex pathophysiology of this disease. Of note, the authors of this review cite a paper stating one third of COPD patients worldwide are nonsmokers. They review how fine particles of smoking induce tissue damage through reactive oxidative stress and inflammation. They also note how pulmonary circulation is altered through endothelial damage. Additionally, they note circulating antibodies against elastin and pulmonary tissue in patients with COPD, and note CD4 cells responding to these tissues. Unfortunately, it is unclear how these processes can be targeted or reversed, but they deepen our understanding of this common disease.
Use of an online crowdfunding platform for unmet financial obligations in cancer care [6]
Unfortunately, the specialization, regionalization, and rapid new advancements of cancer care have added to the “financial toxicity” of cancer diagnosis and treatment. The usage of online crowdfunding has become increasingly prevalent, especially in patients with illness and cancer. This study sought to characterize cancer patients who use crowdfunding, and the nature of their campaigns. They systematically found over 37,000 campaigns, and randomly analyzed 1,035 campaigns. Campaigns often described the patient’s age, employment, diagnosis, and prognosis. Median fundraising goal was $10,000. However, the median total donations obtained was $2,125. Authors found 26% of the campaigns were for those who were underinsured. Limitations included small sample size, inability to verify claims, and possibility for interrater variability, although they noted the interrater reliability exceeded k>0.81.
National trends in utilization and transplantation of HCV-viremic kidneys [7]
Hepatitis C virus (HCV) positive kidneys were often considered undesirable and discarded, and thus not considered for organ transplant. This study analyzed data from 2015-2019 and found that with advances in HCV treatment, transplantation of these organs has increased. With the opioid crisis, the supply of HCV-positive kidneys has increased in recent years. This study also highlights how organ rating systems give HCV-positive kidneys poor ratings, but these kidneys generally function one year after transplant. Despite these advances, many HCV-positive kidneys still get discarded. This study is very promising and interesting.
Dr. Edward T. Carey is a first-year resident physician at NYU Langone Health
Peer reviewed by David Kudlowitz, MD, internal medicine, NYU Langone Health
Image courtesy of Wikimedia Commons
References
[1] Rosenstock, J, Kahn, S, et al. Effect of Linagliptin. Vs Glimepiride on Major Adverse Cardiovascular Outcomes in Patients with Type 2 Diabetes: The CAROLINA Randomized Clinical Trial. JAMA. 2019. 322 (12): 1155-66. https://jamanetwork.com/journals/jama/fullarticle/2751398
[2] Wexler, D. Sulfonyureas and cardiovascular safety: the final verdict? JAMA. 2019. Vol 322. Number 2. 1147-9.
[3] Stone GW, Kappetein AP, Sabik JF, et al., on behalf of the EXCEL Trial Investigators. Five-Year Outcomes After PCI or CABG for Left Main Coronary Disease. N Engl J Med 2019;Sep 28:[Epub ahead of print]. https://www.nejm.org/doi/full/10.1056/NEJMoa1909406
[4] Cheng MP, Stenstrom R, Paquette K, et al, for the FABLED Investigators. Blood Culture Results Before and After Antimicrobial Administration in Patients With Severe Manifestations of Sepsis: A Diagnostic Study. Ann Intern Med. Sept 2019. [Epub ahead of print 17 September 2019.] https://annals.org/aim/article-abstract/2751453/blood-culture-results-before-after-antimicrobial-administration-patients-severe-manifestations
[5] Agusti, A, Hogg, J. Update on the pathogenesis of COPD. NEJM. 2019. 381: 13. 1248-56. https://www.nejm.org/doi/full/10.1056/NEJMra1900475
[6] Cohen, AJ, Brody, H, et al. Use of an online crowdfunding platform for unmet financial obligations in cancer care. JAMA. 2019. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2749759
[7] Potluri, et al. National trends in utilization and transplantation of HCV-viremic kidneys. J Am Soc Nephrology. Oct 2019. 30 (10). 1939-51. https://jasn.asnjournals.org/content/30/10/1939