Peer Reviewed
With medicine advancing at such a rapid pace, it is crucial for physicians to keep up with the medical literature. This can quickly become an overwhelming endeavor given the sheer quantity and breadth of literature released on a daily basis. Primecuts helps you stay current by taking a shallow dive into recently released articles that should be on your radar. Our goal is for you to slow down and take a few small sips from the medical literature firehose.
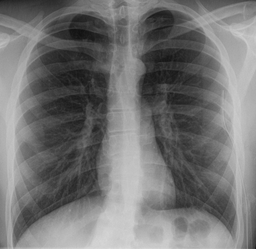
Conservative versus Interventional Treatment for Spontaneous Pneumothorax [1]
Although there exists some diversity in the management of primary spontaneous pneumothorax [2], the most common management involves immediate drainage, typically with chest tube insertion, though surgery is also sometimes needed. Chest tube insertion is often painful, and can lead to organ injury, bleeding, or infection. Meanwhile, conservative observational management is another potential option.
This randomized, multicenter noninferiority trial sought to determine whether or not conservative management of uncomplicated, primary spontaneous pneumothorax is an acceptable alternative to interventional management. A total of 316 patients with moderate-to-large (defined by 32% or more on chest radiography, according to the Collins method [3]) unilateral pneumothorax were randomly assigned to interventional management or conservative management. The primary outcome was defined as radiographic resolution with lung re-expansion at 8 weeks.
The trial found that conservative observational management was noninferior: 98.5% re-expansion with interventional management vs. 94.4% re-expansion with conservative management (95% confidence interval [CI], −8.6–0.5; P=0.02 for noninferiority; prespecified noninferiority margin of -9%). Additionally, conservative observational management resulted in fewer invasive procedures, shorter length of hospital stay, fewer recurrences, and a lower risk of adverse and serious adverse events.
The study offers modest evidence that conservative management is noninferior, especially when considering the implications of the secondary outcomes, but it is also statistically fragile. Data obtained after the 8-week period was treated as “missing” in the original noninferiority statistics. Noninferiority was maintained when the data collection period was extended to 9 weeks, but was not maintained when data “missing” from the original 8-week period was considered by default as treatment failure (i.e. failure of re-expansion).
Current blood pressure guidelines (USPSTF [5], 2017 ACC/AHA [6]) recommend using a mean of multiple blood pressure measurements over time to screen for and manage hypertension in young adults. Despite the understood phenomenon that blood pressure measurements may vary across clinical visits, the clinical relevance of this variability is unknown.
This prospective cohort study involving 3394 African American and Caucasian participants previously enrolled in the Coronary Artery Risk Development in Young Adults (CARDIA) study set out to determine whether long-term, visit-to-visit blood pressure variability from young adulthood to midlife is associated with cardiovascular disease and all-cause mortality by middle age. Data were collected from March 1985 to August 2015, during which patterns of systolic blood pressure were evaluated at year 0 (baseline), and years 2, 5, 7, and 10. The primary outcome was a composite of cardiovascular disease events, including fatal or nonfatal coronary artery disease, hospitalization for heart failure, stroke, and transient ischemic attack.
The study found that greater long-term, visit-to-visit variability from young adulthood to midlife was associated with increased risk for cardiovascular disease and all-cause mortality over the following 20 years. Hazard ratios (accompanied by 95% CI) were reported for mean blood pressure, blood pressure variability independent of the mean, and mean annual change respectively (1.97 [95% CI, 1.77-2.20], 1.44 [1.27-1.63], 1.55 [1.39-1.73]).
These findings suggest that assessment of variability in blood pressure may help identify young adults who are at increased risk later in life. As suggested in the article, programming of electronic medical records to calculate blood pressure variability over time could help healthcare professionals identify individuals at high risk for cardiovascular disease events, as such analysis would otherwise prove quite cumbersome in day-to-day practice.
Post–Acute Kidney Injury Proteinuria and Subsequent Kidney Disease Progression [7]
Acute kidney injury (AKI) has been associated with increased levels of proteinuria after an episode [8,9], and episodes are also associated with more rapid subsequent loss of kidney function. However, studies [10] have shown that only 6% to 17% of patients recently hospitalized with AKI had proteinuria quantified after hospitalization, showing the need for further clarification of the clinical utility of proteinuria quantification.
This multicenter, matched cohort study at four clinical centers in North America enrolled 1538 patients to answer: Among patients who had an AKI, is proteinuria quantified after hospital discharge associated with future loss of renal function? Researchers hypothesized that the level of proteinuria would have a positive correlation with subsequent kidney function loss. The primary outcome was kidney disease progression, defined as either halving of the eGFR or onset of end-stage renal disease.
The study found that higher post-AKI urine albumin-to-creatinine ratio (UACR) was associated with an increased risk of kidney disease progression (HR 1.53; 95% CI 1.45-1.62). This suggests that UACR may be a valuable risk stratification tool, and there should be more widespread and routine quantification of proteinuria after AKI.
There are, however, some limitations. As patients were enrolled following an index hospitalization during which AKI occurred, it is unclear how much of the proteinuria observed 3 months afterward was actually present prior to AKI. Additionally, it has not been assessed whether decreasing proteinuria (with medical management) following AKI would slow rates of kidney disease progression.
Minicuts
This retrospective cohort study explored if an association exists between analogue versus human insulin use with mortality and major cardiovascular events. Researchers analyzed data from 127,600 adults with type 2 diabetes mellitus who had initiated insulin therapy. There were no differences in overall mortality, cardiovascular mortality, hospitalization for heart failure, myocardial infarction or stroke.
Association of Simulated Patient Race/Ethnicity with Scheduling of Primary Care Appointments [12]
This cross-sectional study simulated black, Hispanic, and white patient callers requesting primary care appointments at 804 randomized physician offices in Texas, posing the question of whether belonging to a racial/ethnic minority group is associated with disparities in access. Race and ethnicity of the simulated callers were signaled through their names and voices. The study found that simulated black and Hispanic callers experienced longer wait times (i.e. were offered appointments further in the future) compared to simulated white callers, despite having the same insurance status.
Cost-Effectiveness of Transitional Care Services After Hospitalization with Heart Failure [13]
This study developed a decision analytic microsimulation model to evaluate the lifetime cost-effectiveness of three types of intensive transitional care services (nursing home visits, disease management clinics, and nurse care management) for elderly patients with heart failure discharged from the hospital. The study concluded that transitional care services are economically attractive compared to standard care, with nursing home visits being the most cost-effective service examined. These results suggest that intensive transitional care services should become the new standard of care for this particular population.
Dr. Kyle Ranger Guillory is a first-year resident in internal medicine at NYU Langone Health
Peer reviewed by Christian Torres, MD, chief resident, internal medicine, NYU School of Medicine
Image courtesy of Wikimedia Commons
References
[1] Brown SGA, Ball EL, Perrin K, et al. Conservative versus Interventional Treatment for Spontaneous Pneumothorax. N Engl J Med 2020; 382:405-415. DOI: 10.1056/NEJMoa1910775. https://www.nejm.org/doi/full/10.1056/NEJMoa1910775.
[2] Sahn SA, Heffner JE. Spontaneous pneumothorax. N Engl J Med 2000; 342:868-74. DOI: 10.1056/NEJM200003233421207. https://www.nejm.org/doi/full/10.1056/NEJM200003233421207.
[3] Collins CD, Lopez A, Mathie A, Wood V, Jackson JE, Roddie ME. Quantification of pneumothorax size on chest radiographs using interpleural distances: regression analysis based on volume measurements from helical CT. AJR Am J Roentgenol 1995 Nov; 165(5):1127-1130. DOI: 10.2214/ajr.165.5.7572489. https://www.ajronline.org/doi/10.2214/ajr.165.5.7572489.
[4] Yano Y, Reis JP, Lewis CE, et al. Association of Blood Pressure Patterns in Young Adulthood With Cardiovascular Disease and Mortality in Middle Age. JAMA Cardiol. Published online January 22, 2020. doi:10.1001/jamacardio.2019.5682. https://jamanetwork.com/journals/jamacardiology/fullarticle/2759256.
[5] SiuAL; USPreventiveServicesTaskForce. Screening for high blood pressure in adults: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2015; 163(10):778-786. doi:10.7326/M15-2223. https://annals.org/aim/fullarticle/2456129/screening-high-blood-pressure-adults-u-s-preventive-services-task.
[6] Whelton PK,Carey RM,Aronow WS, et al.2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71(6):e13-e115. doi:10.1161/HYP.0000000000000065. https://www.ahajournals.org/doi/10.1161/HYP.0000000000000065.
[7] Hsu C, Chinchilli VM, Coca S, et al. Post–Acute Kidney Injury Proteinuria and Subsequent Kidney Disease Progression: The Assessment, Serial Evaluation, and Subsequent Sequelae in Acute Kidney Injury (ASSESS-AKI) Study. JAMA Intern Med. Published online January 27, 2020. doi:10.1001/jamainternmed.2019.6390. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2759742.
[8] Parr SK, Matheny ME, Abdel-Kader K, et al. Acute kidney injury is a risk factor for subsequent proteinuria. Kidney Int. 2018; 93(2):460-469. doi:10.1016/j.kint.2017.07.007. https://www.sciencedirect.com/science/article/pii/S0085253817305379?via%3Dihub.
[9] Hsu CY, Hsu RK, Liu KD, et al. Impact of acute kidney injury on urinary protein excretion: analysis of two prospective cohorts (ASSESS-AKI and CRIC). J Am Soc Nephrol. 2019; 30(7):1271-1281. doi:10.1681/ASN.2018101036. https://jasn.asnjournals.org/content/30/7/1271.
[10] Matheny ME, Peterson JF, Eden SK, et al. Laboratory test surveillance following acute kidney injury. PLoS One. 2014; 9(8):e103746. doi:10.1371/journal.pone.0103746. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0103746.
[11] Neugebauer R, Schroeder EB, Reynolds K, et al. Comparison of Mortality and Major Cardiovascular Events Among Adults With Type 2 Diabetes Using Human vs Analogue Insulins. JAMA Netw Open. 2020; 3(1):e1918554. doi:10.1001/jamanetworkopen.2019.18554. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2759275.
[12] Wisniewski JM, Walker B. Association of Simulated Patient Race/Ethnicity With Scheduling of Primary Care Appointments. JAMA Netw Open. 2020; 3(1):e1920010. doi:10.1001/jamanetworkopen.2019.20010. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2759761.
[13] Blum MR, Øien H, Carmichael HL, et al. Cost-Effectiveness of Transitional Care Services After Hospitalization With Heart Failure. Ann Intern Med. 2020; [Epub ahead of print 28 January 2020]. DOI: 10.7326/M19-1980. https://annals.org/aim/fullarticle/2759786/cost-effectiveness-transitional-care-services-after-hospitalization-heart-failure.