Clinical Correlations is proud to present our section for humanism in medicine, Tales From The Bedside, where we showcase our community’s unique and diverse experiences as physicians and trainees in internal medicine.
By Ariella Noorily
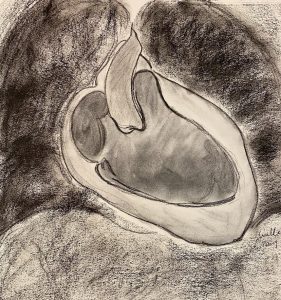 The first time I saw a cardiac MRI, I was sitting in a Kimmel conference room with my firm reviewing the case of a middle-aged woman who presented with atrial fibrillation. We made our way slowly through the data, starting with EKG, then chest X-ray, echocardiogram, chest CT, and labs. Unfortunately, her arrhythmia was not benign—it stemmed from a large atrial angiosarcoma that was growing into the ventricular free wall. I did not have to be familiar with this diagnosis to understand its dismal prognosis: even with all available surgical and medical interventions, the mass would likely kill our patient. Despite this, I heard myself say, “Wow, that’s beautiful,” when the MRI scans appeared on the screen. For a brief moment, the deadly pathology masked itself as a mere component of a work of art, the tumor and pericardial effusion just additional shades of grey within a cardiac silhouette sketched and smudged in charcoal.
The first time I saw a cardiac MRI, I was sitting in a Kimmel conference room with my firm reviewing the case of a middle-aged woman who presented with atrial fibrillation. We made our way slowly through the data, starting with EKG, then chest X-ray, echocardiogram, chest CT, and labs. Unfortunately, her arrhythmia was not benign—it stemmed from a large atrial angiosarcoma that was growing into the ventricular free wall. I did not have to be familiar with this diagnosis to understand its dismal prognosis: even with all available surgical and medical interventions, the mass would likely kill our patient. Despite this, I heard myself say, “Wow, that’s beautiful,” when the MRI scans appeared on the screen. For a brief moment, the deadly pathology masked itself as a mere component of a work of art, the tumor and pericardial effusion just additional shades of grey within a cardiac silhouette sketched and smudged in charcoal.
This tendency to separate our patients from their diseases is common in our profession, and I have experienced it many times since starting clerkships. My friends often describe their cases as “wild,” “interesting,” “exciting,” “smelly,” “unbelievable,” or “perfect for learning everything there is to know about heart failure.” At rounds, my attendings comment on the most “fascinating” cases and bring me to press the most edematous legs, palpate the largest goiters, look at the craziest CT scans, and listen to the best murmurs, crackles, and bruits. I reciprocate with my own stories about the belly that drained ten liters of ascitic fluid and the heart that I could see beating behind a cachectic chest wall.
At times, we let ourselves forget that the impressive crackles come from the lungs of a woman whose diffuse scleroderma is preventing her from traveling home to her husband and children in Ghana. We may revel in the excitement of witnessing our first abdominal paracentesis without considering the woman beneath the needle, who began drinking when her husband started hitting her. We watch a cardiac apex rhythmically reappear through the ribs of a grown man who weighs less than I do because of the lung cancer that is quickly spreading into his bones, glands, and spirit. I then marvel at the beauty of the cardiac MRI, though the scan predicts the death of an unsuspecting woman with a newly diagnosed angiosarcoma.
I often allow the technicalities of a case to stimulate my mind before I become emotionally attached to a patient. Perhaps I developed this defense mechanism in order to survive working in a profession that is constantly tossing us between joy and sadness, from depression to exhilaration—a profession that I chose exactly for the wide array of feelings that I now struggle to manage. I have found myself tuning into interesting physical exam findings and beautiful images so that these emotions do not take over.
Still, all of the most impressive murmurs and crackles mean much less without the names or stories that bring them to life. The challenge of medicine is to find a way for the objective data and the human connection to blend so seamlessly that they resemble components of one work of art: each lab value, personal story, exam finding, and emotion another shade of grey within the heart of the piece.
Ariella Noorily is a third-year medical student at NYU Grossman School of Medicine. She is part of the three-year track for Diagnostic Radiology, and will be starting her internship at NYU Langone Health in July.