Peer Reviewed
A 68-year-old woman with a history of hypertension and well controlled type 2 diabetes presents to the ED with five days of progressively worsening dyspnea on exertion, orthopnea, and bilateral leg swelling. Prior to this episode, she complained of having a cold for a few days, which has since resolved. Her physical exam is notable for bibasilar crackles and 1+ bilateral lower extremity edema to her knees. She is admitted for a presumed heart failure exacerbation. During her admission, she is treated with IV lasix with subsequent resolution of her symptoms. Her echo demonstrates an ejection fraction of 45%. Should she be discharged solely with a maintenance diuretic for heart failure with preserved ejection fraction? Should she be started on guideline-directed medical therapy for heart failure with reduced ejection fraction? Does she even qualify for either of these categories? Does it matter?
Physicians love to classify. We love categories and sub-categories, which expand and change in conjunction with our ever-growing knowledge of various areas of medicine. The evolution of the classes of heart failure and their respective names exemplifies this. Congestive heart failure was first differentiated into systolic and diastolic heart failure, which were further re-classified as heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). How did that happen and, perhaps more importantly, why?
In 1933, heart failure was defined as “a condition in which the heart fails to discharge its contents adequately” [1]. This definition, while vague, reiterates the fact that heart failure is a clinical syndrome characterized by common symptoms of congestion caused by a failing of the heart to expel its volume adequately, making its diagnosis all the more complex. In 1965, Dr. Stuart Bartle used the term “ejected fraction,” to describe the ratio of stroke volume to end diastolic volume [2]. Despite the introduction of this new term, congestive heart failure was the predominant label given to patients with clinical signs and symptoms of heart failure in the 1980s to 1990s [3]. However, clinicians began to recognize that a significant proportion of patients with clinical heart failure had normal left ventricular ejection fractions; these patients were largely categorized as having diastolic heart failure [4]. Early heart failure clinical trials included patients with a range of ejection fractions [18-20]. However a higher mortality rate observed with lower ejection fraction subgroups drove subsequent trials to exclude patients with higher ejection fractions in order to calculate more practical sample sizes [21-23]. In 2013, the ACC/AHA Guideline for the Management of Heart Failure formally defined HFrEF as having an ejection fraction less than or equal to 40% and HFpEF as having an ejection fraction greater than or equal to 50% [5]. These new guidelines created an intermediate, unaccounted for, group of patients with ejection fractions between 41 and 49%, leading the way for the birth of “the middle child of heart failure” – heart failure with mid-range ejection fraction (HFmrEF) [6]. This category was first thought to solely represent milder systolic dysfunction, and then was formally adopted as an independent category in the 2016 European Society of Cardiology Heart Failure Guidelines [7].
The rise of HFmrEF is accompanied by numerous questions, all of which seem to boil down to one: What does this mean for our patients? To begin to answer that question, investigators are doing what is done to all middle children – comparing them to their siblings. The hope is that understanding how HFmrEF is similar or distinct from HFrEF and HFpEF will shed light on its development, management, and prognosis. Even this, however, is wrought with difficulties. First, HFpEF is still quite an ambiguous category with no evidence-based therapies as of yet [6]. Second, patients with HFmrEF have been excluded from the large heart failure trials [7]. Therefore, much of the data on HFmrEF are extrapolated from HFrEF or HFpEF trials that included patients with ejection fractions of 40-50%, are retrospective studies, or are observational studies – studies that thus introduce unaccounted-for biases and confounding variables. Given how relatively young this category of heart failure is, there are also no longitudinal studies that follow the progression of HFmrEF. Stemming from the lack of longitudinal data, there is still debate surrounding whether HFmrEF is a distinct clinical entity or merely a transition zone between HFrEF and HFpEF [7]. In a study from Washington University School of Medicine, 168 patients with documented HFmrEF were identified from a heart failure registry and researchers determined whether their ejection fractions were improved, worsened, or the same from roughly two to four years prior. The authors found that 73% of the HFmrEF patients had improved ejection fractions following the initiation of guideline-directed medical therapy for HFrEF, 17% had worsened, and 10% were unchanged [8].
Is HFmrEF, then, just an intermediate class? The Get With The Guidelines – Heart Failure (GWTG-HF) registry of hospitalized heart failure patients provided the largest cohort of HFmrEF patients thus far [9,10]. This was a prospective, observational study involving almost 100,000 heart failure patients across 305 hospitals, 13% of whom had HFmrEF. From this cohort, researchers found that the demographics of HFmrEF patients were similar to HFpEF patients; HFmrEF patients were older with a median age of 77 years and more likely female compared to those with HFrEF [10]. Also similar to HFpEF, the HFmrEF group had higher rates of co-morbidities, most notably diabetes and atrial fibrillation, than seen in HFrEF [10]. Notably, this is in contrast to other studies that have found that HFmrEF patients were more similar to HFrEF patients in regards to these characteristics, demonstrating inconsistencies in the data available [6]. However, more than two-thirds of HFmrEF patients had a history of ischemic heart disease; this high prevalence of coronary artery disease is consistent among studies and is a striking similarity between HFmrEF and HFrEF [10]. Interestingly, a study found that the transition from HFpEF to HFrEF was more likely in patients with a history of myocardial infarction [11]. HFmrEF has also been found to be more similar to HFrEF in imaging markers of adverse cardiac remodeling [12]. This raises the possibility that HFmrEF patients are potentially not only those recovering from HFrEF, but also HFpEF patients with coronary artery disease who are deteriorating into HFrEF [9]. With this possibility comes the separate question of the significance of coronary artery disease in the prognosis of HFpEF and, more pertinently, the question of what therapies should then be offered to patients with HFmrEF to perhaps prevent its progression to HFrEF. It also raises the larger question of whether ejection fraction is an adequate biomarker for categorizing the subtypes of heart failure.
Post-hoc analyses of randomized controlled trials analyzing the effects of guideline-directed medical therapy for HFrEF, namely ARBs and spironolactone, on HFpEF have demonstrated that patients with ejection fractions on the lower end of the spectrum tended to have better outcomes with these classes of medications [13, 14, 15]. These were patients who would now be classified as HFmrEF. To more directly assess the use of guideline-directed medical therapy in HFmrEF, a study involving 1,144 HFmrEF patients in Korea admitted for acute heart failure exacerbations discharged these patients with a beta-blocker, renin-angiotensin system blocker (RASB), or aldosterone antagonist [16]. There were significantly lower rates of all-cause mortality in patients discharged with a beta-blocker and in those discharged with a RASB compared to their respective controls after two years post-discharge [16]. Although this study found no significant difference in outcome when patients were discharged with or without an aldosterone antagonist, a recent prospective study found that, among patients with HFmrEF, spironolactone use upon discharge was associated with a significant reduction in the composite of all-cause death or heart failure readmission [16,17]. Along a similar line, the PARAGON-HF trial studied the use of Entresto in HFpEF patients [24]. While there was no significant difference in hospitalizations and cardiovascular mortality, it did suggest potential benefit in those with ejection fractions of 45-57% [24]. These studies yet again raise the question of whether HFmrEF is a distinct category or one that includes multiple etiologies of heart failure – some which respond to guideline-directed medical therapy, and some that do not.
While HFmrEF rivals its sibling, HFpEF, in terms of complexity and the number of questions surrounding its core features, a great deal of work has been done to make the waters less muddy. It is still unclear whether HFmrEF is simply a period of transition when patients are either recovering their ejection fractions or progressing from HFpEF to HFrEF due to underlying coronary artery disease or other disease processes. What is clearer, however, is the prevalence of ischemia in HFmrEF and its potential contribution to deterioration of ventricular function. This potential has motivated studies that demonstrate the likely benefit of guideline-directed medical therapy for our patients who live in this grey zone with ejection fractions between 41 and 49%, allowing us to better counsel and, hopefully, treat them.
Dr. Pamela Boodram is a chief resident in the NYU Langone Internal Medicine Residency
Peer reviewed by Bernard Kadosh, MD, assistant professor, Department of Medicine (Division of Cardiology)
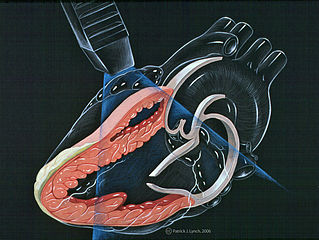
Image courtesy Wikimedia Commons
References
- Lewis T. Diseases of the Heart. 1st ed. London, United Kingdom: MacMillian; 1933.
- Bartle SH, Sanmarco ME, Dammann JF. Ejected Fraction: An Index of Myocardial Function (abstr.). Am J Cardiol. 1965;15(1):1.
- Pfeffer, M, Shah AM, Borlaug BA. Heart Failure With Preserved Ejection Fraction In Perspective. Circ Res. 2019;124:1598-1617. https://doi.org/10.1161/CIRCRESAHA.119.313572
- Gaasch, WH and Zile MR. Left Ventricular Diastolic Dysfunction and Diastolic Heart Failure. Annual Review of Medicine 2004 55:1, 373-394. https://doi.org/10.1146/annurev.med.55.091902.104417
- Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/ American Heart Association task force on practice guidelines. Circulation. 2013;128(16):e240–327. https://doi.org/10.1161/CIR.0b013e31829e8776
- Lam CS and Solomon SD. The Middle Child in Heart Failure: Heart Failure with Mid-Range Ejection Fraction (40-50%). Eur J Heart Fail. 2014;16(10):1049–55. https://doi.org/10.1002/ejhf.159
- Srivastava, PK, Hsu, JJ, Ziaeian, B, Fonarow, GC. Heart Failure with Mid-Range Ejection Fraction. Curr Heart Fail Rep (2020). https://doi.org/10.1007/s11897-019-00451-0
- Rastogi A, Novak E, Platts AE, Mann DL. Epidemiology, Patho-physiology and Clinical Outcomes for Heart Failure Patients with a Mid-Range Ejection Fraction. Eur J Heart Fail. 2017;19(12):1597–1605. https://doi.org/10.1002/ejhf.879
- Lam CSP, Teng TK. Understaning Heart Failure with Mid-Range Ejection Fraction. JACC. 2016;4(6):473-476. http://dx.doi.org/10.1016/j.jchf.2016.03.025
- Kapoor JR, Kapoor R, Ju C, et al. Precipitating Clinical Factors, Heart Failure Characterization, and Outcomes in Patients Hospitalized with Heart Failure with Reduced, Borderline, and Preserved Ejection Fraction. JACC. 2016;4(6):464-472. http://dx.doi.org/10.1016/j.jchf.2016.02.017
- Clarke CL, Grunwald GK, Allen LA, et al. Natural history of left ventricular ejection fraction in patients with heart failure. Circ Cardiovasc Qual Outcomes 2013;6:680–6. https://doi.org/10.1161/CIRCOUTCOMES.111.000045
- Doeblin PJ, Pieske B, Kelle S, et al. v HFmEF Differs From HFpEF and HFrEF in Advanced CMR Imaging Markers of Adverse Cardiac Remodeling. Circulation. 2018;138:A13417. https://www.ahajournals.org/doi/10.1161/circ.138.suppl_1.13417
- Lund LH. Heart Failure with Mid-Range Ejection Fraction: Lessons from CHARM. Cardiac Failure Review. 2018;4(2):70–2. https://doi.org/10.15420/cfr.2018.11.2
- Pitt B, Pfeffer MA, Assmann SF, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med 2014; 370: 1383–1392. https://doi.org/10.1056/NEJMoa1313731
- Solomon SD, Claggett B, Lewis EF, et al. Influence of ejection fraction on outcomes and efficacy of spironolactone in pa- tients with heart failure with preserved ejection fraction. Eur Heart J 2016; 37: 455–462. https://doi.org10.1093/eurheartj/ehv464
- Choi KH, Choi JO, Jeon ES, et al. Guideline-Directed Medical Therapy for Patients With Heart Failure With Midrange Ejection Fraction: A Patient-Pooled Analysis From the KorHF and KorAHF Registries. J Am Heart Assoc. 2018;7: e009806. https://doi.org/10.1161/JAHA.118.009806
- Enzan N, Matsushima S, Ide T, et al. Spironolactone use is associated with improved outcomes in heart failure with mid-range ejection fraction. ESC Heart Failure. 2020. https://doi.org/10.1002/ehf2.12571
- Cohn JN, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a Veterans Administration Cooperative Study. N Engl J Med. 1986; 314:1547-1552. Doi: 10.1056/NEJM19860612314204
- CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study. N Engl J Med. 1987; 316: 1429-35.
- Cohn JN, et al. The V-HeFT Study. Veterans Administration Cooperative Study Group. Circulation. 1990; 81: III48-III53.
- Cohn JN, et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med. 1991; 325: 303-310. Doi:10.1056/NEJM199108013250502
- Yusuf S, et al. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991; 325: 293-302. Doi: 10.1056/NEJM199108013250501
- Pitt B, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999; 341: 709-717. Doi: 10.1056/NEJM199909023411001
- Solomon SD, et al. Angiotensin-Neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019; 318: 1609-1620. DOI: 10.1056/NEJMoa1908655