Peer Reviewed
Your next patient is very familiar. The management of her chronic diseases–heart failure (HF) and chronic kidney disease (CKD)—has been optimized. Like the 6.2 million other Americans with HF1 and the 37 million Americans with CKD,2 practice guidelines have recommended several medications to minimize the risk of disease progression.
In the practice of medicine, much time is spent persuading patients that the new medication being prescribed is vital for continued good health or future survival. For a patient with HF and CKD, there is perhaps no class of medication where this argument is truer than the renin-angiotensin-aldosterone system (RAAS) inhibitors. These medications–angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARB), and mineralocorticoid receptor antagonists (MRA)–have been established as particularly important for patients with heart failure with reduced left ventricular ejection fraction (HFrEF), with numerous studies demonstrating their efficacy in reducing hospitalization and mortality.3-9
But perhaps the endorsement of the American College of Cardiology and American Heart Association regarding the cardioprotective, blood pressure lowering benefits of these medications is not a compelling enough selling point for your medication-averse patient. You can confidently tell your patient that this prescription is handling two birds with one stone: a RAAS inhibitor just so happens to be a frontline medication for slowing the progression of their declining kidney function.10-18
Having reminded yourself and the patient of the importance of these medications, you find yourself suddenly given pause while reviewing recent laboratory results: a potassium level of 5.5 mEq/L. On the backfoot now, you are considering a difficult question: For your patient with HF and/or CKD, how can we balance the many benefits of RAAS inhibitors against their risk of exacerbating hyperkalemia?
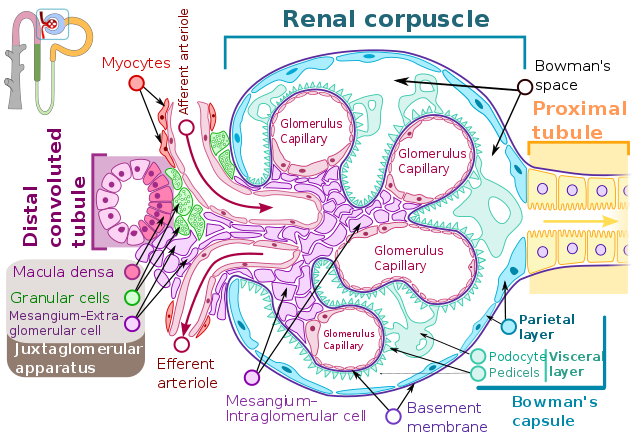
Hyperkalemia frequently complicates adherence to guideline-recommended RAAS inhibition for patients with HFrEF and CKD.19-22 RAAS inhibitors elevate potassium levels by suppressing aldosterone secretion by the adrenal glands, downstream from renin secretion. Aldosterone normally promotes the activity of epithelial sodium channels (ENaC) in the renal collecting tubules, which promotes potassium wasting through an increased electrochemical gradient, driving potassium out through renal outer medullary potassium (ROMK) channels.23 In patients controlled on RAAS inhibitors, the risk of hyperkalemia must be weighed against the risk of undertreated disease. Hyperkalemia, particularly when resulting from acute elevations, can manifest as severe muscle weakness/paralysis,24 cardiac conduction abnormalities/arrhythmias,25 and metabolic acidosis via impaired renal ammonium excretion.26 Due to concern for these potentially fatal complications, advanced kidney disease with refractory hyperkalemia is an indication for initiating kidney replacement therapy (KRT).27 A nationwide Swedish observational study of over 10,000 individuals suggested that continuation of RAAS inhibitors in the setting of end-stage kidney disease (ESKD) was associated with an increased absolute risk of KRT.28 Analysis of Danish National registries also revealed an association between elevated all-cause mortality and potassium levels over 5.0 mEq/L.29
None of this is to say that the decision to reduce or discontinue these medications in the setting of hyperkalemia is a completely satisfactory solution. Stopping RAAS medications following incident hyperkalemia has been associated with an increased mortality risk in patients admitted for acute heart failure,30 and subgroup analysis of the EMPHASIS-HF study examining patients at high risk for hyperkalemia on the aldosterone antagonist eplerenone has demonstrated preservation of mortality benefit.31 Further support for the lifesaving cardioprotective effects of these medications has been seen in two large observational studies showing decreased 5-year cardiac event and mortality rates in CKD patients maintained on RAAS inhibitors in advanced kidney disease compared to those in whom the medication was withdrawn.28,32
With this delicate balance of risk and benefit in mind, the standard approach to minimize the risk of hyperkalemia has historically been fourfold:
- Reduction of dietary potassium to <2-3 g/day; sources include fruits, vegetables, meats, nuts, and cereals.33
- Use of potassium-wasting thiazide and loop diuretics.33 Potassium-wasting diuretics are appropriate for management of blood pressure in CKD; higher doses are likely to be required.
- Addition of alkali, which may increase K excretion and slow the progression of CKD when metabolic acidosis is present.34
- Reduction in therapeutic RAAS inhibition, as follows: Reduce the dose if K >5.5 mEq/L, stop if K >6.0 mEq/L, until K ≤5.0 mEq/L.35
When facing the unsatisfactory decision to reduce or limit uptitration of effective therapy, there is reason to consider adding instead of subtracting medications and starting one of the promising new potassium-binding agents to boost gastrointestinal potassium excretion.
While the first potassium-binding agent, sodium polystyrene sulfonate (Kayexalate®, Concordia Pharmaceutical, St. Michael, Barbados), was approved in 1958 for the emergent treatment of hyperkalemia through cation exchange for sodium in the GI tract, its tolerability has been limited by this resin’s propensity for volume expansion following water absorption, with risk for bowel obstruction and colonic necrosis.36 Fortunately, newer medications including patiromer (Veltassa®, Vifor Pharma, Zurich, Switzerland; $50.37/8.4g unit, FDA-approved 2015) and sodium zirconium cyclosilicate (SZC, Lokelma®, AstraZeneca, Cambridge, UK; $28.33/5g unit, FDA-approved 2018) have demonstrated promise as cation exchangers with favorable side effect profiles.
Patiromer effectively exchanges potassium in the distal colon for calcium as a means of increasing gastrointestinal potassium excretion, without evidence of volume expansion predisposing to obstruction.37 Patiromer has demonstrated efficacy in reducing the incidence of hyperkalemia (7.3% vs 24.5% placebo), as well as allowing more successful uptitration of spironolactone during four-week treatment in patients with a history of hyperkalemia prompting discontinuation of RAAS inhibitors or CKD with GFR <60 mL/min.38
SZC utilizes sodium exchange for potassium throughout the GI tract. The HARMONIZE clinical trial data revealed a low side-effect burden with 29 days of use, and a return to normokalemia within 48 hours for 98% of participants with a mean potassium of 5.6 mEq/L.39
Given the tolerability and efficacy suggested by these studies, providers caring for HF and CKD patients who are benefiting from RAAS inhibitor therapy should follow further study of these drugs closely, as they represent a promising new solution to an all-too-common high-stakes clinical dilemma.36,40-42 Barriers to widespread adoption of these agents include high cost, a lack of studies demonstrating mortality benefit, and that they come as powders that need to be dissolved in water.
Logan Groneck is a 2nd year medical student at NYU Grossman School of Medicine
Reviewed by David Goldfarb, MD, Professor, Department of Medicine, Neuroscience and Physiology, NYU Grossman School of Medicine, Chief Nephrology, NY Harbor VA Medical Center
Image courtesy of Wikimedia Commons, source:[File:Renal corpuscle-en.svg|Renal_corpuscle-en], Author-Shypoetess
References
- Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139-596. https://www.ahajournals.org/doi/10.1161/CIR.0000000000000757
- Centers for Disease Control and Prevention. Chronic kidney disease in the United States, 2021. Centers for Disease Control and Prevention website. Published 2021. Updated March 4, 2021. Accessed April 29, 2021 https://www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html
- Yancy CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. 2016;68:1476–1488. https://www.sciencedirect.com/science/article/pii/S0735109716330248?via%3Dihub
- Granger CB, McMurray JJV, Yusuf S, et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function intolerant to angiotensin-converting-enzyme inhibitors: the CHARM– Alternative trial. 2003;362(9386):772–776. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(03)14284-5/fulltext
- Cohn JN, Tognoni G; Valsartan Heart Failure Trial Investigators. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345(23):1667–1675. https://www.nejm.org/doi/full/10.1056/NEJMoa010713
- Zannad F, McMurray JJV, Krum H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364(1):11–21. https://www.nejm.org/doi/full/10.1056/NEJMoa1009492
- Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation study investigators. N Engl J Med. 1999;341(10):709–717. https://www.nejm.org/doi/full/10.1056/NEJM199909023411001
- Pfeffer MA, Braunwald E, Moyé LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction: results of the survival and ventricular enlargement trial. The SAVE investigators. N Engl J Med. 1992;327(10):669–677. https://www.nejm.org/doi/full/10.1056/NEJM199209033271001
- SOLVD Investigators, Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. The SOLVD Investigators. N Engl J Med. 1991;325:293–302 https://www.nejm.org/doi/10.1056/NEJM199108013250501
- Kidney Disease: Improving Global Outcomes. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):1-150. https://kdigo.org/wp-content/uploads/2017/02/KDIGO_2012_CKD_GL.pdf
- Xie X, Liu Y, Perkovic V, et al. Renin-angiotensin system inhibitors and kidney and cardiovascular outcomes in patients with CKD: a Bayesian network meta-analysis of randomized clinical trials. Am J Kidney Dis. 2016;67(5):728-741. https://www.ajkd.org/article/S0272-6386(15)01312-8/fulltext
- The GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia): Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy. Lancet. 1997;349(9069):1857–1863. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(96)11445-8/fulltext
- Brenner BM, Cooper ME, de Zeeuw D, et al.; RENAAL Study Investigators. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–869. https://www.nejm.org/doi/full/10.1056/NEJMoa011161
- Jafar TH, Schmid CH, Landa M, et al.: Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease. A meta-analysis of patient-level data. Ann Intern Med. 2001;135(2):73–87. https://www.acpjournals.org/doi/10.7326/0003-4819-135-2-200107170-00007
- Kent DM, Jafar TH, Hayward RA, et al.: Progression risk, urinary protein excretion, and treatment effects of angiotensin-converting enzyme inhibitors in nondiabetic kidney disease. J Am Soc Nephrol. 2007;18(6):1959–1965. https://jasn.asnjournals.org/content/18/6/1959.long
- Lewis EJ, Hunsicker LG, Clarke WR, et al.; Collaborative Study Group: Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345(12):851–860. https://www.nejm.org/doi/full/10.1056/NEJMoa011303
- Maschio G, Alberti D, Janin G, et al. Effect of the angiotensin-converting-enzyme inhibitor benazepril on the progression of chronic renal insufficiency. The Angiotensin-Converting-Enzyme Inhibition in Progressive Renal Insufficiency Study Group. N Engl J Med. 1996;334(15):939–945. https://www.nejm.org/doi/full/10.1056/NEJM199604113341502
- Ruggenenti P, Perna A, Gherardi G, Gaspari F, Benini R, Remuzzi G. Renal function and requirement for dialysis in chronic nephropathy patients on long-term ramipril: REIN follow-up trial. Gruppo italiano di Studi Epidemiologici in Nefrologia (GISEN). Ramipril Efficacy In Nephropathy. 1998;352(9136):1252–1256. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(98)04433-X/fulltext
- Palmer BF. Managing hyperkalemia caused by inhibitors of the renin-angiotensin-aldosterone system. N Engl J Med. 2004;351(6):585–592. https://www.nejm.org/doi/full/10.1056/NEJMra035279
- Reardon LC, Macpherson DS. Hyperkalemia in outpatients using angiotensin-converting enzyme inhibitors. How much should we worry? Arch Intern Med. 1998;158(1):26–32. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/190873
- Sarwar CMS, Papadimitriou L, Pitt B, et al. Hyperkalemia in heart failure. J Am Coll Cardiol. 2016;68(14):1575–1589. https://doi.org/10.1016/j.jacc.2016.06.060
- Yildirim T, Arici M, Piskinpasa S, et al. Major barriers against renin-angiotensin-aldosterone system blocker use in chronic kidney disease stages 3-5 in clinical practice: a safety concern? Ren Fail. 2012;34(9):1095–1099. https://www.tandfonline.com/doi/full/10.3109/0886022X.2012.717478
- Rossi GM, Regolisti G, Peyronel F, Fiaccadori E. Recent insights into sodium and potassium handling by the aldosterone-sensitive distal nephron: a review of the relevant physiology and drug discovery. J Nephrol. 2020;33(3):431-445. https://link.springer.com/article/10.1007/s40620-019-00684-1
- Finch CA, Sawyer CG, Flynn JM. Clinical syndrome of potassium intoxication. Am J Med. 1946;1:337-352. https://www.amjmed.com/article/0002-9343(46)90052-6/pdf
- Mattu A, Brady MJ, Robinson DA. Electrocardiographic manifestations of hyperkalemia.” Am J Emerg Med. 2000;18(6):721-729. https://doi.org/10.1053/ajem.2000.7344
- Karet FE. Mechanisms in hyperkalemic renal tubular acidosis. J Am Soc Nephrol. 2009;20(2):251-254. https://jasn.asnjournals.org/content/20/2/251.long
- van de Luijtgaarden MWM, Noordzij M, Tomson C, et al. Factors influencing the decision to start renal replacement therapy: results of a survey among European nephrologists. Am J Kidney Dis. 2012;60(6):940–948. https://www.ajkd.org/article/S0272-6386(12)01027-X/fulltext
- Fu EL, Evans M, Clase CM, et al. Stopping renin-angiotensin system inhibitors in patients with advanced CKD and risk of adverse outcomes: a nationwide study. J Am Soc Nephrol. 2021;32(2):424-435. https://jasn.asnjournals.org/content/32/2/424.long
- Aldahl M, Jensen AC, Davidsen L, et al. Associations of serum potassium levels with mortality in chronic heart failure patients. Eur Heart J. 2017;38(38):2890–2896. https://academic.oup.com/eurheartj/article/38/38/2890/4082641
- Beusekamp JC, Tromp J, Cleland JGF, et al. Hyperkalemia and treatment with RAAS inhibitors during acute heart failure hospitalizations and their association with mortality. JACC Heart Fail. 2019;7(11): 970-979. https://doi.org/10.1016/j.jchf.2019.07.010
- Eschalier R, McMurray JJ, Swedberg K, et al. Safety and efficacy of eplerenone in patients at high risk for hyperkalemia and/or worsening renal function: analyses of the EMPHASIS-HF study subgroups (Eplerenone in Mild Patients Hospitalization And SurvIval Study in Heart Failure). J Am Coll Cardiol. 2013;62(17):1585-1593. https://doi.org/10.1016/j.jacc.2013.04.086
- Palmer BF. Potassium binders for hyperkalemia in chronic kidney disease– diet, renin-angiotensin-aldosterone system inhibitor therapy, and hemodialysis. Mayo Clin Proc. 2020;95(2):339-354. https://www.mayoclinicproceedings.org/article/S0025-6196(19)30486-0/pdf
- Goraya N, Wesson DE. Management of the metabolic acidosis of chronic kidney disease. Adv Chronic Kidney Dis. 2017;24(5):298-304. https://www.ackdjournal.org/article/S1548-5595(17)30094-0/fulltext
- Kovesdy CP. Management of hyperkalaemia in chronic kidney disease. Nat Rev Nephrol. 2014;10(11):653-662. https://www.nature.com/articles/nrneph.2014.168
- DeFilippis EM, Desai AS. Treatment of hyperkalemia in heart failure. Curr Heart Fail Rep. 2017;14(4):266-274. https://doi.org/10.1007/s11897-017-0341-0
- Sterns RH, Grieff M, Bernstein PL. Treatment of hyperkalemia: something old, something new. Kidney Int. 2016;89(3):546–554. https://www.kidney-international.org/article/S0085-2538(15)00123-4/fulltext
- Pitt B, Anker SD, Bushinsky DA, Kitzman DW, Zannad F, Huang IZ; PEARL-HF Investigators. Evaluation of the efficacy and safety of RLY5016, a polymeric potassium binder, in a double-blind, placebo-controlled study in patients with chronic heart failure (the PEARL-HF) trial. Eur Heart J. 2011;32(7):820-828. https://academic.oup.com/eurheartj/article/32/7/820/2398451
- Kosiborod M, Rasmussen HS, Lavin P, et al. Effect of sodium zirconium cyclosilicate on potassium lowering for 28 days among outpatients with hyperkalemia: the HARMONIZE randomized clinical trial. JAMA. 2014;312(21):2223-2233. https://jamanetwork.com/journals/jama/fullarticle/1936753
- Colbert GB, Patel D, Lerma EV. Patiromer for the treatment of hyperkalemia. Expert Rev Clin Pharmacol. 2020;13(6):563-570. https://www.tandfonline.com/doi/abs/10.1080/17512433.2020.1774363?journalCode=ierj20
- Takkar C, Nassar T, Qunibi W. An evaluation of sodium zirconium cyclosilicate as a treatment option for hyperkalemia. Expert Opin Pharmacother. 2021;22(1):19-28. https://www.tandfonline.com/doi/abs/10.1080/14656566.2020.1810234?journalCode=ieop20
- Llubani R, Vukadinović D, Werner C, Marx N, Zewinger S, Böhm M. Hyperkalaemia in heart failure–Pathophysiology, implications and therapeutic perspectives. Curr Heart Fail Rep. 2018;15(6):390-397. https://doi.org/10.1007/s11897-018-0413-9