Peer Reviewed
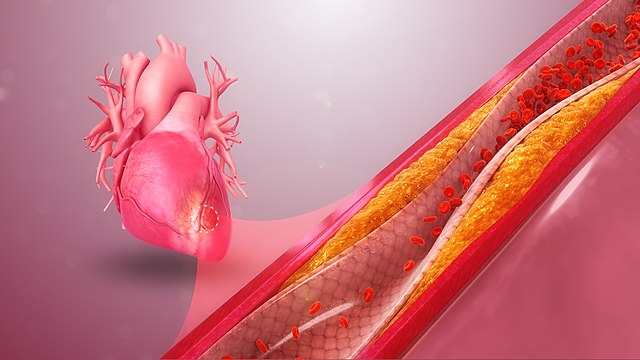
First developed in 1990,1 coronary artery calcium scoring has emerged as a noninvasive risk stratification tool for the detection of atherosclerotic cardiovascular disease (ASCVD).2 Unlike other commonly used cardiovascular risk stratification tools based on clinical, epidemiological, and laboratory features,3-4 the coronary artery calcium score (CACS) is a direct and reliable marker of calcified plaque burden in the epicardial coronary arteries.2 The CACS may aid in the accurate estimation of a patient’s 10-year ASCVD risk, which is used to determine initiation of statin therapy for primary prevention of cardiovascular disease.5-6 However, the clinical utility of the CACS remains.
The CACS is attained via rapidly acquired, non-contrast computed tomography of the heart.7 The radiation exposure is comparable to mammography8 and each scan costs around $100.7 The Agatston method is widely used to calculate the calcium score; the area of each calcified lesion is multiplied by a density-weighting factor and then summed to obtain the total score.1 A score of zero corresponds to no identifiable disease. Scores of 1-99, 100-399, and ≥400 Agatston units correspond to mild, moderate, and severe disease, respectively.1
The prognostic value of the CACS has been extensively studied via longitudinal, prospective studies. The largest of these, the Multi-Ethnic Study of Atherosclerosis (MESA), included over 6000 asymptomatic men and women without known cardiovascular disease. The study found the CACS to be a powerful, independent predictor of future cardiac events.9 At 10 years of follow-up, the rate of cardiovascular events, including myocardial infarction, stroke, cardiac arrest, and cardiac-related deaths, was <5% in those with CAC scores of zero and >7.5% in those with CAC scores ≥100.9 Incorporating the CACS with traditional cardiovascular risk factors results in a high reclassification rate among patients with intermediate ASCVD risk.10-11 Moreover, the CACS is the strongest predictor of future cardiovascular events compared to other nontraditional markers of cardiovascular disease, including ankle-brachial index and C-reactive protein.12 Despite this, the role of the CACS is controversial13-15 and clinical practice guidelines for using the score as a risk stratification tool for primary prevention are inconsistent.5,16
Current American College of Cardiology (ACC) and American Heart Association (AHA) guidelines recommend CAC scans for patients in whom evidence of coronary calcium may change statin treatment and risk factor modification (recommendation class IIb).5 Specifically, it is recommended in asymptomatic adults ≥40 years of age with intermediate 10-year ASCVD risk (7.5-19.9%). It may be useful in some patients with borderline risk (5-7.5%) as well.5 It is not recommended in patients with low (<5%) or high (≥20%) 10-year ASCVD risk, as the CACS is unlikely to change treatment approach in these patients.5 Other patient populations that may benefit from knowing their coronary artery calcium score include patients reluctant to initiate or reinstitute statin therapy, and older patients with low risk factor burden who question the utility of initiating statin therapy.5
The score can be incorporated with traditional risk factors using the MESA risk score calculator,17 refining the patient’s estimated 10-year ASCVD risk and aiding in decision-making regarding risk reduction and statin therapy. For patients with CAC scores ≥100 or ≥75th percentile for age and gender, therapeutic lifestyle changes, aggressive risk factor modification, and statin therapy are recommended, independent of other cardiovascular risk factors. In patients with a CACS of zero, it is considered safe to defer statin therapy with reassessment in 5-10 years. There are no specific recommendations for patients with scores between 1-99, although statins can be considered based on patient and provider shared decision-making.5
In contrast, the US Preventive Services Task Force (USPSTF) found insufficient evidence (“I” grade) to support the routine use of the CACS in asymptomatic adults to prevent cardiovascular events.16 In the report, they acknowledge that adding CACS to various risk stratification tools resulted in an improved reclassification of patients in the intermediate risk cohort, although the clinical significance of these changes is unknown. Given the low incidence of cardiovascular events in the general population, they maintained that many patients would be inappropriately reclassified to a higher risk category. Moreover, randomized control trials are lacking. In two randomized trials that investigated the effect on clinical outcomes of incorporating the CACS into traditional risk stratification tools, there was no significant difference in cardiovascular events at four years.18-19 The USPSTF assessment acknowledges many other potential disadvantages of CAC scans, including exposure to ionizing radiation (albeit relatively low) and the potential for false positives leading to subsequent diagnostic procedures such as stress testing and coronary angiography (although two studies investigating a downstream increase in cardiac testing and procedures had conflicting findings).20-21 Other potential downsides to the routine use of CACS include the inability to rule out non-calcified plaque, incidental findings, increased patient anxiety, and repeat testing, amplifying concerns about radiation exposure.22
The USPSTF assessment of 2018 was met with numerous responses defending the clinical utility of CAC scoring, maintaining that the harms are small in magnitude, and emphasizing its potential to improve patient adherence. For instance, studies have found a positive correlation between CACS and statin adherence.23-24 While the cost-effectiveness of CAC scoring also remains controversial, most studies conclude that performing CAC scans according to the 2018 ACC/AHA guidelines is cost-effective when the use of daily statin therapy is considered to significantly affect patient quality of life.25-26 When taken in the context of other routinely performed screening tests, such as screening colonoscopies in asymptomatic patients aged 45-74, CACS may be equivalent in terms of cost-effectiveness.
Lastly, the absence of calcium on imaging is the strongest negative predictor of cardiovascular disease, termed “the power of zero.”27 With the risk of gastrointestinal bleeding in patients treated with aspirin and up to 20% of patients on statin therapy reporting myalgias,22 a CACS of zero has the potential to avoid unintended adverse consequences related to the use of statins and aspirin in patients unlikely to benefit.13
In conclusion, evidence supports a high CACS as a strong positive predictor of cardiovascular events; however, it is still unclear which patient groups should undergo coronary artery CT scanning to guide clinical decision-making. Ultimately, the value of the CACS is both physician- and patient-dependent: only scores with the potential to modify pharmacologic therapy or risk- reduction strategies will prove useful. For physicians who widely encourage the use of statin therapy and aggressive risk reduction, the CACS may be of no added benefit. Conversely, for physicians or patients more averse to the potential adverse effects and cost burden of statins, the CACS may be useful as part of a risk-benefit discussion regarding their initiation. Nevertheless, further research is needed to discern the true ability of the CACS to improve patient outcomes as a risk-stratifying tool for the primary prevention of cardiovascular events, with hopes of ending the ongoing debate and further elucidating optimal CACS screening practices.
By Kyla Wright is a 2nd year medical student at NYU Grossman School of Medicine
Reviewed by Adam Skolnick, MD, cardiology, NYU Langone Health
Image courtesy of Wikimedia Commons, source: http://www.scientificanimations.com/
References
- Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827-832. https://pubmed.ncbi.nlm.nih.gov/2407762/
- Cheong BYC, Wilson JM, Spann SJ, Pettigrew RI, Preventza OA, Muthupillai R. Coronary artery calcium scoring: an evidence-based guide for primary care physicians. J Intern Med. 2021;289(3):309-324. https://pubmed.ncbi.nlm.nih.gov/33016506/
- Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S49-73. https://pubmed.ncbi.nlm.nih.gov/24222018/4
- Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837-1847. https://pubmed.ncbi.nlm.nih.gov/9603539/5
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082-e1143. https://pubmed.ncbi.nlm.nih.gov/30565953/
- US Preventive Services Task Foirce, Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;316(19):1997-2007. https://pubmed.ncbi.nlm.nih.gov/27838723/
- Hecht HS. Coronary artery calcium scanning: past, present, and future. JACC Cardiovasc Imaging. 2015;8(5):579-596. https://pubmed.ncbi.nlm.nih.gov/25937196/
- Voros S, Rivera JJ, Berman DS, et al. Guideline for minimizing radiation exposure during acquisition of coronary artery calcium scans with the use of multidetector computed tomography: a report by the Society for Atherosclerosis Imaging and Prevention Tomographic Imaging and Prevention Councils in collaboration with the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr. 2011;5(2):75-83. https://pubmed.ncbi.nlm.nih.gov/21398199/
- Budoff MJ, Young R, Burke G, et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: the multi-ethnic study of atherosclerosis (MESA). Eur Heart J. 2018;39(25):2401-2408. https://pubmed.ncbi.nlm.nih.gov/29688297/
- Erbel R, Mohlenkamp S, Moebus S, et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol. 2010;56(17):1397-1406. https://pubmed.ncbi.nlm.nih.gov/20946997/
- McClelland RL, Jorgensen NW, Budoff M, et al. 10-Year Coronary Heart Disease Risk Prediction Using Coronary Artery Calcium and Traditional Risk Factors: Derivation in the MESA (Multi-Ethnic Study of Atherosclerosis) With Validation in the HNR (Heinz Nixdorf Recall) Study and the DHS (Dallas Heart Study). J Am Coll Cardiol. 2015;66(15):1643-1653. https://pubmed.ncbi.nlm.nih.gov/26449133/
- Yeboah J, McClelland RL, Polonsky TS, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA. 2012;308(8):788-795. https://pubmed.ncbi.nlm.nih.gov/22910756/
- McEvoy JW, Martin SS, Blaha MJ, et al. The case for and against a coronary artery calcium trial: Means, motive, and opportunity. JACC Cardiovasc Imaging. 2016;9(8):994-1002. https://pubmed.ncbi.nlm.nih.gov/27491486/
- Ebell MH. Should family physicians use coronary artery calcium scores to screen for coronary artery disease? No: screening is unproven, expensive, and potentially harmful. Am Fam Physician. 2012;86(5):405-406. https://pubmed.ncbi.nlm.nih.gov/22963058/
- Greenland P, Blaha MJ, Budoff MJ, Erbel R, Watson KE. Coronary calcium score and cardiovascular risk. J Am Coll Cardiol. 2018;72(4):434-447. https://pubmed.ncbi.nlm.nih.gov/30025580/
- Lin JS, Evans CV, Johnson E, Redmond N, Coppola EL, Smith N. Nontraditional risk factors in cardiovascular disease risk assessment: Updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2018;320(3):281-297. https://pubmed.ncbi.nlm.nih.gov/29998301/
- The Multi-Ethnic Study of Atherosclerosis. MESA 10-year CHD risk with coronary artery calcification. Published 2021. Accessed June 12th, 2021. www.mesa-nhlbi.org/MESACHDRisk/MesaRiskScore/RiskScore.aspx.
- Rozanski A, Gransar H, Shaw LJ, et al. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the EISNER (Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research) prospective randomized trial. J Am Coll Cardiol. 2011;57(15):1622-1632. https://pubmed.ncbi.nlm.nih.gov/21439754/
- Arad Y, Spadaro LA, Roth M, Newstein D, Guerci AD. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin C, and vitamin E: the St. Francis Heart Study randomized clinical trial. J Am Coll Cardiol. 2005;46(1):166-172. https://pubmed.ncbi.nlm.nih.gov/15992652/
- Shreibati JB, Baker LC, McConnell MV, Hlatky MA. Outcomes after coronary artery calcium and other cardiovascular biomarker testing among asymptomatic Medicare beneficiaries. Circ Cardiovasc Imaging. 2014;7(4):655-662. https://pubmed.ncbi.nlm.nih.gov/24777939/
- Chi WC, Sylwestrzak G, Barron J, Kasravi B, Power T, Redberg R. Does CAC testing alter downstream treatment patterns for cardiovascular disease? Am J Manag Care. 2014;20(8):e330-339. https://pubmed.ncbi.nlm.nih.gov/25295796/
- Fernandez G, Spatz ES, Jablecki C, Phillips PS. Statin myopathy: a common dilemma not reflected in clinical trials. Cleve Clin J Med. 2011;78(6):393-403. https://pubmed.ncbi.nlm.nih.gov/21632911/
- Kalia NK, Miller LG, Nasir K, Blumenthal RS, Agrawal N, Budoff MJ. Visualizing coronary calcium is associated with improvements in adherence to statin therapy. Atherosclerosis. 2006;185(2):394-399. https://pubmed.ncbi.nlm.nih.gov/16051253/
- Taylor AJ, Bindeman J, Feuerstein I, et al. Community-based provision of statin and aspirin after the detection of coronary artery calcium within a community-based screening cohort. J Am Coll Cardiol. 2008;51(14):1337-1341. https://pubmed.ncbi.nlm.nih.gov/18387433/
- Spahillari A, Zhu J, Ferket BS, et al. Cost-effectiveness of contemporary statin use guidelines with or without coronary artery calcium assessment in African American individuals. JAMA Cardiol. 2020;5(8):871-880. https://pubmed.ncbi.nlm.nih.gov/32401264/
- Hong JC, Blankstein R, Shaw LJ, et al. Implications of coronary artery calcium testing for treatment decisions among statin candidates according to the ACC/AHA cholesterol management guidelines: a cost-effectiveness analysis. JACC Cardiovasc Imaging. 2017;10(8):938-952. https://pubmed.ncbi.nlm.nih.gov/28797417/
- Blaha MJ, Cainzos-Achirica M, Greenland P, et al. Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: The Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2016;133(9):849-858. https://pubmed.ncbi.nlm.nih.gov/26801055/