Peer Reviewed
With October beginning and the weather starting to change, the season for apple picking, Pumpkin Spice Lattes, and football also commences. However, with all the joys of fall, we also begin flu season and prepare for all the complications that it brings. With this in mind, we turn to the medical literature which searches for novel treatments for this deadly illness.
Oseltamivir, Amantadine and Ribavirin Combination Antiviral Therapy versus Oseltamivir Monotherapy for the Treatment of Influenza
The flu is a very costly and dramatic illness, and the new seasonal vaccine is just coming out. Oseltamivir is our only line of defense after disease onset, and it reduces the typical one to two-week disease course by approximately one day if given properly [1]. There have also been some studies showing it reduces the risk of acquiring other lower respiratory tract infections and other hospital complications [2]. While those results are somewhat promising there is still much to be desired for such a common and costly disease. Many other viruses have been targeted with combination antiviral therapy. Previously, the combination of amantadine, oseltamivir and ribavirin has shown increased antiviral activity (maximizing effective drug concentration) of each of these drugs in vitro compared to each of the drugs independently. Additionally, this combination can be used even if treatment is delayed for 72 hours compared to the 24-48 hour window recommended for oseltamivir monotherapy.
So, with hopes of finding a better treatment solution for influenza, a randomized double-blind phase 2 study was conducted on 560 patients across 5 countries [3] comparing combination amantadine, oseltamivir and ribavirin versus oseltamivir monotherapy. The study showed a 10% absolute reduction in viral shedding on day 3 as well as significant viral load reduction with combination therapy. By day 7, viral shedding was similar in combination versus monotherapy. Most importantly, and to the dismay of researchers, there was no significant clinical benefit in terms of fevers, myalgia, respiratory symptoms, etc. when comparing the two groups. The combination group did however experience more serious adverse events (GI and respiratory), though it is unclear if that can be contributed to the therapy. In preclinical trials, a decreased viral load and shedding has been associated with decreased symptoms but only in animal models, and the combination therapy shows decreased shedding compared to monotherapy. However, the US Food and Drug Administration does not believe this should be considered as it does not appropriately assess how well a patient “feels, functions or survives.” With decreased viral load and thus, viral shedding, may come other benefits like decreased resistance and decreased infectivity. Ultimately, the search for a symptomatic resolution for influenza continues, and whether it will be a combination or a novel medication remains to be seen. In the meantime, make sure to get vaccinated.
Continuous Glucose Monitoring versus Usual Care in Patients with Type 2 Diabetes
Recently, continuous glucose monitoring (CGM) has been popular in treating Type 1 diabetes. It sends glucose values to patients’ cell phones every 5 minutes. A sensor is placed in subcutaneous fat, and measures glucose in interstitial fluid. Patients can observe how their body is responding to insulin and assess what foods or activities help keep their diabetes under control. Studies have shown CGM can reduce A1C by about 0.6% points compared to regular care (over 24 weeks), and it has been suggested that it can be helpful in monitoring hypoglycemia as well [4]. This is fairly impressive given that no medication is required and it also gives patients autonomy over their glucose levels.
However, CGM has not been studied with Type 2 diabetes, thus a 24-week trial across North America was conducted to do so [5].  The study initially enrolled 254 participants, but lost 93 of them to withdrawal and ineligibility. Half of the participants were given the CGM system and training on how to use the CGM as an adjunct to regular blood glucose monitoring. The control group did not receive a CGM device, but were asked to monitor blood glucose 4 times daily with adjustments to medications being left to the discretion of patients’ individual providers. Biochemical hypoglycemia was infrequent across both groups. Mean HbA1C reduction was 0.8% in CGM vs. 0.5% in control, with an improvement of 0.3% (95% CI of 0.5 to 0.0). This improvement is less than what was seen in Type 1 diabetics, and it is postulated that patients with Type 2 diabetes have less advanced diabetes management skills (carb counting and experience since youth) which limits the value of CGM, but these findings do suggest that CGM could be useful. Though the paper suggests beginning to use CGM now, another study of a larger sample size may be appropriate to better assess the benefit and also obtain satisfaction data to assess if patients felt the CGM offered a greater feeling of control on their diabetes management.
IVIg for Treatment of Severe Refractory Heparin-Induced Thrombocytopenia
Heparin Induced Thrombocytopenia (HIT) is a common and frightening concern when a patient receiving heparin experiences a drop in platelets. Unfortunately, repleting platelets can be dangerous (can double rates of mortality [6]) and finding an alternative anticoagulant is dangerous as patients are already thrombocytopenic, but we cannot ignore the possibility of DVTs, strokes, CAD and other embolic complications. With such high mortality and no great solution, further research is warranted to search for creative options.
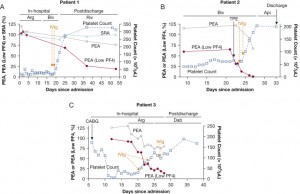
A recent paper published in Chest [7] reported on three patients with severe HIT refractory to standard therapy but who had sustained response to IVIG. One patient, a 47-year-old man, had a PE and right atrial thrombus 13 days after heparin administration. He received argatroban, thrombectomy and multiple platelet transfusions along with dexamethasone and bivalirudin, but he maintained severely thrombocytopenic for 2.5 weeks until being given 1g/kg per day on 2 consecutive days. He remained free of thrombocytopenia for 8 months following this period. A second patient, 9 days after receiving heparin for CABG, became thrombocytopenic and suffered from a pulmonary embolus. This patient remained thrombocytopenic for 3 weeks despite platelet transfusion and therapeutic plasma exchange. He also was given IVIG and remained free of thrombosis and thrombocytopenia for 7 months. The third patient also had persistently low platelets and DVTs 5 days after CABG and heparin exposure, and for 2 weeks he remained thrombocytopenic despite normal care. With IVIG, he too improved. In these cases, the timeline between sustained response and complementary laboratory data “leave little doubt” that there is some causal relationship between the IVIG and clinical improvement. The figure below shows these patients’ platelet response to IVIG. There may be some patients with particular genotypes that lend resistance to IVIG usage, but for the most part the study suggests implementing the use of IVIG for HIT response. This data warrants prospective trials to better assess the utility of IVIG for those with refractory HIT. Importantly though, IVIG can be procoagulable for certain patients [8] and more data is needed to ensure this could be a safe solution to a very complex problem of HIT.
Weight and Metabolic Outcomes 12 years after Gastric Bypass
Obesity is a costly epidemic in our country. A recent study suggested even healthy obese people in this country can amount to tens of thousands of dollars in healthcare costs solely for their risk of developing more significant disease [9]. Surgery and gastric bypass have been effective in maintaining weight-loss and improving type 2 diabetes, but there is little comprehensive data on long-term follow-up of Roux-en-Y bypasses.
An observational prospective study was initiated in July 2000 through March 2016 involving 1156 patients [10] where ultimately 835 patients were followed, and about half (418) had surgery while the other 417 did not. There was also a population-based sample of 321 adults who were recruited separately but had not undergone surgery or been seen at the surgical center (i.e. not seeking surgery). The study compared these three groups, looking at weight lost, remission rates of Type 2 diabetes, hypertension and dyslipidemia 12 years after surgery. The mean percentage weight loss was persistent at 12 years (26.9%) for the surgical group as compared with 0.9-2% mean percentage weight loss in the non-surgery groups. Type 2 diabetes remission was 75% at 2 years, 62% at 6 years and 51% at 12 years in this study in the surgical group. However, in subgroup analysis, this benefit was weaker in patients who had initiated insulin therapy before receiving their bypass. This indicates a less significant impact if Type 2 Diabetes is more advanced prior to surgery. Similar results were seen in a Swedish study.
Of note, there were 7 deaths by suicide (5 in the surgery group and 2 in the non-surgery group). It is unclear why those suicides occurred and whether it is related to the surgery and the lifestyle that follows. More studies need to be conducted to evaluate and determine the need for close mental health follow-up for patients receiving bariatric surgery. Despite the low risk (<2%) for suicide compared to general population, it does appear that bariatric surgery has substantial health benefits in the way of diabetes and weight loss that are sustained for at least 12 years.
On that note, we will go to some MiniCuts:
Turns out exercise is good for your body. The PURE study looked at the exercise patterns of 130,000 people. People who exercise intensely have 13% less mortality and 9.5% less major CAD events which is better than most medication [11].
JAMA looked at the associations between healthcare costs and being on Supplemental Nutrition Assistance Programs (SNAP). They found savings of approximately $1400 in healthcare per year in regards to ED visits compared to patients with similar socioeconomic statuses (200% below the poverty level) who did not receive SNAPÂ [12]. For even more intensive information on the parallels between social spending and health care costs, check out the book, The American Health Care Paradox by Elizabeth Bradley.
A study in Gastroenterology investigated Proton Pump Inhibitors (PPIs) and their association with CKD development [13]. They found that PPI users had a Hazard Ratio of 1.26 (95% CI of 1.05 to 1.51) in developing CKD with higher degrees of ESRD and AKI compared to H2 Blocker users. These were modest results, but continue to add more reasons to reduce the use of chronic PPI use.
Dr. Kumar Vasudevan, a 2nd year Internal Medicine Resident at NYU Langone Health
Peer reviewed by Dana Zalkin, MD, 3rd year Internal Medicine Resident, NYU Langone Health
Image courtesy of Wikimedia Commons
References:
- Cooper Nicola J, Sutton Alexander J, Abrams Keith R, Wailoo Allan, Turner David, Nicholson Karl G et al. Effectiveness of neuraminidase inhibitors in treatment and prevention of influenza A and B: systematic review and meta-analyses of randomized controlled trialsBMJ 2003; 326 :1235 http://www.bmj.com/content/326/7401/1235.long
- Hernán MA, Lipsitch M. Oseltamivir and Risk of Lower Respiratory Tract Complications in Patients with Flu Symptoms: A Meta-analysis of Eleven Randomized Clinical Trials. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2011; 53(3):277-279. https://www-ncbi-nlm-nih-gov/pmc/articles/PMC3137795/
- Beigel, John et al. Oseltamivir, amantadine, and ribavirin combination antiviral therapy versus oseltamivir monotherapy for the treatment of influenza: a multicentre, double-blind, randomized phase 2 trial. Lancet. 2017. thelancet.com/journals/laninf/article/PIIS1473-3099(17)30476-0/fulltext
- Beck RW, Riddlesworth T, Ruedy K, Ahmann A, Bergenstal R, Haller S, et al DIAMOND Study Group Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections: the DIAMOND randomized clinical trial.JAMA2017317371378 http://jamanetwork.com.ezproxy.med.nyu.edu/journals/jama/fullarticle/2598770
- Beck RW, Riddlesworth TD, Ruedy K, Ahmann A, Haller S, Kruger D, et al. Continuous Glucose Monitoring Versus Usual Care in Patients With Type 2 Diabetes Receiving Multiple Daily Insulin Injections: A Randomized Trial. Ann Intern Med. 2017; 167:365–374.doi: 10.7326/M16-2855. http://annals.org/aim/article/2649297/continuous-glucose-monitoring-versus-usual-care-patients-type-2-diabetes
- Padmanabhan A, Jones C, et al. IVIG for Treatment of Severe Refractory Heparin-Induced Thrombocytopenia. Chest. Vol 152 Is 3. September 2017. p 478 – 485. https://www-sciencedirect-com/science/article/pii/S0012369217307249#bib40
- M. Ammann, M.P. Jones, B.K. Link, et al. Intravenous immune globulin and thromboembolic adverse events in patients with hematologic malignancy Blood, 127 (2) (2015), pp. 200-207 http://www.bloodjournal.org/content/127/2/200.long?sso-checked=true
- Norton, Amy. US pays high price for Obesity. CBS News. September 2017. https://www.cbsnews.com/news/us-pays-high-price-for-obesity/
- Adams T, Davidson L, Litwin S et al. Weight and Metabolic Outcomes 12 Years after Gastric Bypass. New England Journal of Medicine. September 21, 2017. 377:1143-1155. http://www.nejm.org/doi/full/10.1056/NEJMoa1700459#t=article
- Lear S, Hu W, Rangarajan S et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. The Lancet. September 2017. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(17)31634-3/fulltext
- Berkowitz SA, Seligman HK, Rigdon J, Meigs JB, Basu S. Supplemental Nutrition Assistance Program (SNAP) Participation and Health Care Expenditures Among Low-Income Adults. JAMA Intern Med.Published online September 25, 2017. doi:10.1001/jamainternmed.2017.4841 http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2653910?amp;utm_source=JAMA%20Intern%20MedPublishAheadofPrint&utm_campaign=25-09-2017
- Klatte DCF, Gasparini A, Xu H et al. Association between Proton Pump Inhibitor Use and Risk of Progression of Chronic Kidney Disease. Gastroenterology. Vol 153 Issue 3. September 2017 p 638-640. https://www-sciencedirect-com/science/article/pii/S0016508517356883