 By Maria Garcia-Jimenez, MD/MHS, Abinav Baweja, MD, and Nicole LaNatra, MD
By Maria Garcia-Jimenez, MD/MHS, Abinav Baweja, MD, and Nicole LaNatra, MD
Peer Reviewed
Clinical vignette
A 65-year old woman with history of invasive breast cancer presents to her primary care provider for regular follow up. She was diagnosed with breast cancer over 10 years ago and received chemotherapy, radiation, and hormonal therapy with aromatase inhibitors. She follows with several providers including an oncologist, surgical oncologists, and a gynecologist. In your clinic, she reports concerns of neuropathy and arthralgia, and mentions that since retiring she worries more about a cancer recurrence and potential financial burdens of additional cancer-related medical care. You wonder what role you can play in her care and how to address her concerns.
(Adapted from Nekhlyudov L. Cancer Survivorship E-Learning Series for Primary Care Providers. George Washington University Cancer Institute module: Cancer Survivors in Primary Care)
The case above underscores several issues pertinent to cancer survivors and what is uniquely called cancer survivorship care – First, what defines a cancer survivor? What are the needs of cancer survivors? Why is cancer survivorship care important in the current healthcare landscape? As this patient population continues to grow, the need to increase education and training in cancer survivorship care becomes more pertinent at all stages of medical training. This article aims to spark awareness for cancer survivorship by presenting evidence behind the needs of cancer survivors and the unique challenges in organizing a survivorship clinic.
A. Who are cancer survivors?
The term “cancer survivor” did not enter medical lexicon until the 1980s, motivated by efforts from the National Coalition for Cancer Survivorship (1). At that time the definition included an individual from “the time of diagnosis through the balance of his or her life.” Family members and caregivers were also included in the definition as they too are impacted by the cancer experience. More recently “cancer survivor†refers to an individual who has completed both treatment for cancer and a period of surveillance monitoring, which typically approximates 5 years after diagnosis (2). In this regard, the term is critical in setting apart this patient population, highlighting their unique medical and psychosocial needs, and shaping national guidelines behind their delivery.
B. Cancer survivors in the United States are a vulnerable growing population that warrant special attention
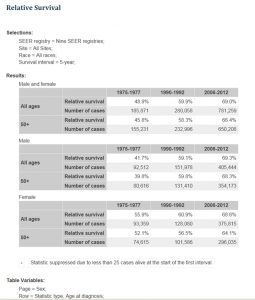
The American Cancer Society (ACS) estimates that at least 15.5 million individuals in the United States are survivors of cancer, and this figure is estimated to encroach on 20 million by 2026 (2). Notably, 47% of cancer survivors are 70 years or older, and 5% are younger than 40. With ongoing advancements in cancer screening, diagnostics, and therapies these numbers are expected to increase at an exceptional rate (Table 1).
The 2005 Institute of Medicine report, “From Cancer Patient to Cancer Survivor: Lost in Transition,†emphasized that a lack of definitive guidance exists on what constitutes best practices in caring for survivors. The lack of guidelines contributes to wide variations across the nation in the care of cancer survivors (2, 3, 4). Much of this variability is related to how new this field is, compounded by the psychosocial and medical issues innate to cancer patients. This large and dynamic patient cohort thus calls for adult providers – both specialists and generalists – to be better equipped in the care of cancer survivors.
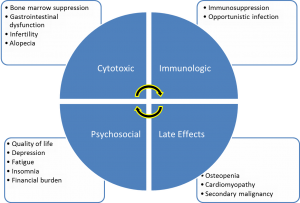
C. Cancer survivors face many long-term health consequences directly from their malignancy and secondary to its treatment
Having a personal history of cancer is an independent risk factor for poor health and disability, and greater limitations in activities of daily living (ADLs) and independent ADLs (5). Cancer survivors often have pre-existing comorbidities and are at increased risk for long-term disability or premature mortality, directly related to their cancer and cytotoxic therapies (4, 6). Examples of cancer and treatment-related morbidity include lymphedema, sexual dysfunction, cognitive impairment, obesity, chronic pain, and fatigue (Figure 1) (5, 7). In one study of approximately 800 U.S. cancer survivors, 2/3 reported concerns of fatigue and loss of strength, while about 50% of them reported sleep difficulties and sexual dysfunction (8, 9). In fact, insomnia is 2-3 times more prevalent in cancer survivors compared to healthy adults (9). In a study of 752 patients diagnosed with one of the ten most common cancers, sleep difficulties (47.9%), sexual dysfunction (41.2%), and concerns of physical health (67.1%) remained pervasive issues (10). When compared to the general population, these issues stood out even up to 10 years after completion of treatment (7, 10), which falls well into what one considers the “survivorship period.†The prevalence of depression among cancer survivors in the US is 3-5 times greater than in the general population (8). Lastly, a population based nationally representative study found a higher incidence and risk of obesity in people with a history of cancer compared to those without. In their study of 32,447 cancer survivors, Greenlee et al. observed an increase in the prevalence of obesity from 22.4% to 31.7% in cancer survivors and from 20.9% to 29.5% in adults without a history of cancer (P < .001, both groups) (11). In subgroup analyses, colorectal, breast, and non-Hispanic black cancer survivors experienced higher annual percent changes in obesity prevalence. Importantly, while these long-term sequelae diminish quality of life, they can be addressed by focused survivorship care geared towards education, targeted screening, prevention, and intervention (6).
D. Why is increasing awareness and implementation of survivorship care important?
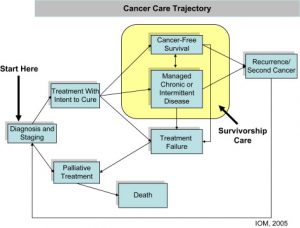
A significant body of knowledge exists about the effects of pediatric cancers and their treatment on adult survivors of pediatric cancers; however, the same is not true for survivors of adult cancers (12). As time from an initial cancer diagnosis elapses, survivors are more likely to receive care from their primary care providers. Those with multiple comorbidities tend to receive care from multiple providers as well (4). Despite the access to well-focused primary and specialized care, these providers may not be equipped to screen for various late effects attributed to prior cancer treatments. An example is best seen in therapy-induced cardiomyopathy, a potentially irreversible side effect of breast cancer and acute leukemia treatments (e.g. the monoclonal antibody-trastuzumab as well as the anthracyclines-daunorubicin, idarubicin, respectively). Their effect on depressed left ventricular function can manifest acutely or several years after therapy (13). While the toxic effects cannot be abrogated completely, treatment of underlying heart failure with evidence-based medications (beta blockers, angiotensin-converting enzyme inhibitors) is beneficial to a patient’s cardiovascular health. Although a primary care physician may know that a patient was treated for a remote cancer, he or she may not be apt to screening for such a toxic effect. This may be a function of knowledge and training, but also related to not being guided or communicated through the oncologist. Though such a skillset is in the realm of the oncologist, it needs to be shared with all providers. Raising awareness to transfer this knowledge to general practitioners is imperative to detecting patients at risk for such late toxicity. Beyond awareness, the development of standardized criteria within a survivorship clinic to implement screening and testing of late and more immediate effects will benefit this patient population. Because no uniform standards for this exist, significant efforts will be required to understand the needs of survivors and to delineate concrete models of comprehensive, coordinated care that meet those needs (Figure 2). With the advent of newer immunotherapeutics (monoclonal and bispecific antibody conjugates), targeted kinase inhibitors, and multi-modal therapeutic strategies, a need for coordinated care between primary care physicians and oncologists is even greater.
E. What models exist for survivorship care? What about at Bellevue Hospital Center?
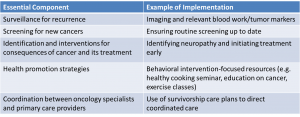
As a relatively new field in medical care, survivorship is crucial in addressing the multitude of chronic and potentially debilitating issues experienced by adult cancer survivors. The American Society for Clinical Oncology (ASCO), in accordance with key recommendations from the Institute of Medicine (IOM), has led the way in proposing models, guidelines, and recommendations for survivorship care in an effort to establish quality care standards (12). While various models of survivorship care exist – from multi-disciplinary based care within a cancer center, to one-time consultations by an oncologist in academic centers, to a shared care model involving primary care providers – the feasibility and efficacy are primarily dependent on available resources, and no evidence exists on the efficacy of the various models (10, 12). Central to the shared care model supported by ASCO and the IOM, is a “survivorship care plan” (SCP) (4, 7, 12). The SCP is developed by the oncologist and provided to the survivor and the survivor’s PCP for the continuation of long-term care. The SCP includes details about cancer treatment, potential long term and late effects of treatment, recommended surveillance for recurrence and late effects, and information on psychosocial support resources (1, 14). It serves as a guideline for addressing IOM-identified components of survivorship care – surveillance of primary malignancy, management of latent complications of cancer treatment, reduction of risks for second malignancies, assessment of psychosocial functioning and coordination of care with a primary care physician (Table 2).
Though there is no evidence supporting a single model of cancer survivorship care, studies have shown that cancer survivors receiving care from a primary care provider and an oncologist are more likely to be up-to-date on cancer-related and non-cancer related preventive services (10, 12). To improve the quality of survivorship care, and empower and educate patients and primary care providers, Bellevue Hospital Center has developed a Cancer Survivorship Clinic. The aim of the clinic is to provide cancer survivors: A. Attention to late effects of cancer treatment (fatigue, insomnia, pain), B. Access to genetic counseling and testing, C. Education on their cancer history and prior treatment, D. Resources on nutrition, exercise, and weight-management (physical therapy, healthful cooking/food seminars), and E. Enhanced awareness and access to resources for survivorship related issues (outreach groups, social support programs). In a shared care model, a SCP is completed during each patient’s first visit. Through the SCP primary care providers and oncologists can communicate, standardize, and coordinate comprehensive care for each survivor; all while increasing awareness and support of cancer survivorship issues. With multiple services available to the survivorship provider and patient, the Bellevue Cancer Survivorship Clinic is unique in empowering patients not only with the knowledge but with the skills to effect behavioral changes to maintain resiliency as survivors.
Conclusions
The patient experience of cancer diagnosis, treatment, and post treatment care is life altering, and life-long. This health care trajectory is encompassed in the idea of cancer survivorship. With improved screening and therapeutics, the cancer survivor population is becoming more prevalent within our healthcare environment. As we reflect on the case presented above, we can appreciate the unique challenges faced by cancer survivors. These include long-term health issues; namely a multitude of side effects which have biologic, psychosocial, and financial toxicities. This presents an opportunity to incorporate primary care providers with specialists as integral members of cancer survivor care. While several resources are available for survivors, concerted efforts to increase education and awareness among medical trainees will be imperative in order to effect changes that will benefit cancer survivors.
Maria Garcia-Jimenez, MD/MHS, Abinav Baweja, MD, and Nicole LaNatra, MD, Bellevue Hospital Center, 462 1st Avenue, New York, NY 10016, Department of Internal Medicine, Department of Hematology/Oncology, Bellevue Cancer Survivorship Clinic, 462 1st Avenue, New York, NY 10016
Peer reviewed by Susan Talbot, MD, Medicine, NYU Langone Health
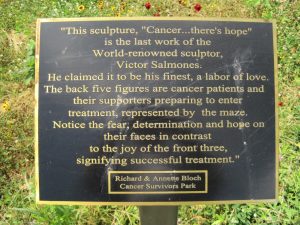
Image courtesy of Wikimedia commons
References:
- Ganz, P. Survivorship: Adult Cancer Survivors. Primary Care Clinical Office Practice. 2009. 36; 721-741.
- Mayer, DK., Nasso, SF., et al. Defining cancer survivors, their needs, and perspectives on survivorship health care in the USA. Lancet Oncology. 2017.
- Hewitt M et al. (2003). Cancer survivors in the United States: age, health, and disability. J Gerontol A Biol Sci Med Sci. 58(1): 82-91.
- From Cancer Patient to Cancer Survivor: Lost in Transition. Institute of Medicine Report Recommendations. 2005.
- Weaver, KE. Reeve, FLP., et al. Mental and physical health-related quality of life among US cancer survivors: population estimates from the 2010 National Health Interview Survey. Cancer Epidemiology Biomarkers Prev. 21(11): 2108-2117.
- Cancer Treatment & Survivorship Facts & Figures 2016-2017. American Cancer Society.
- McCabe MS, Jacobs LA. (2012). Clinical Update: Survivorship Care – Models and Programs. Seminars in Oncology Nursing. 28 (3): e1-e8.
- Ganz, P., Coscarelli, A., et al. (1996). Breast cancer survivors: psychosocial concerns and quality of life. Breast Cancer Research and Treatment. 38.
- Irwin, MR., Olmstead, RE., et al. (2013). Sleep disturbance, inflammation, and depression risk in cancer survivors. Brain, Behavior, and Immunity. 30.
- Baker, F., Denniston, M., Smith, T., et al. (2005). Adult Cancer Survivors: How are they faring? Cancer. 1(104).
- Greenlee, H., Shi, Z., et al. (2016). Trends in obesity prevalence in adults with a history of cancer: Results from the US national health interview survey, 1997 to 2014. J Clin Oncol. 34(26):3133-40.
- McCabe, MS., Bhatia, S., et al. (2013). American Society of Clinical Oncology Statement on high quality cancer survivorship care. Journal of Clinical Oncology. 5(31).
- Volkova M, Russel R. Anthracycline cardiotoxicity: prevalence, pathogenesis and treatment. Curr Cardiol Rev. 2011; 7(4): 214–220
- Ganz PA, Casillas J, Hahn EH. (2008). Ensuring Quality Care for Cancer Survivors: Implementing the Survivorship Care Plan. Seminars in Oncology Nursing. (24):3; 208–217
Tables/Figures:
Table 1: Relative Survival and Number of Cases for all Cancers 1975-2012 (SEER Database)
Figure 1: Toxicities of Cancer and Treatment
Figure 2: Cancer Survivorship: Where does it fit in?