Podcast: Play in new window | Download
Subscribe: RSS
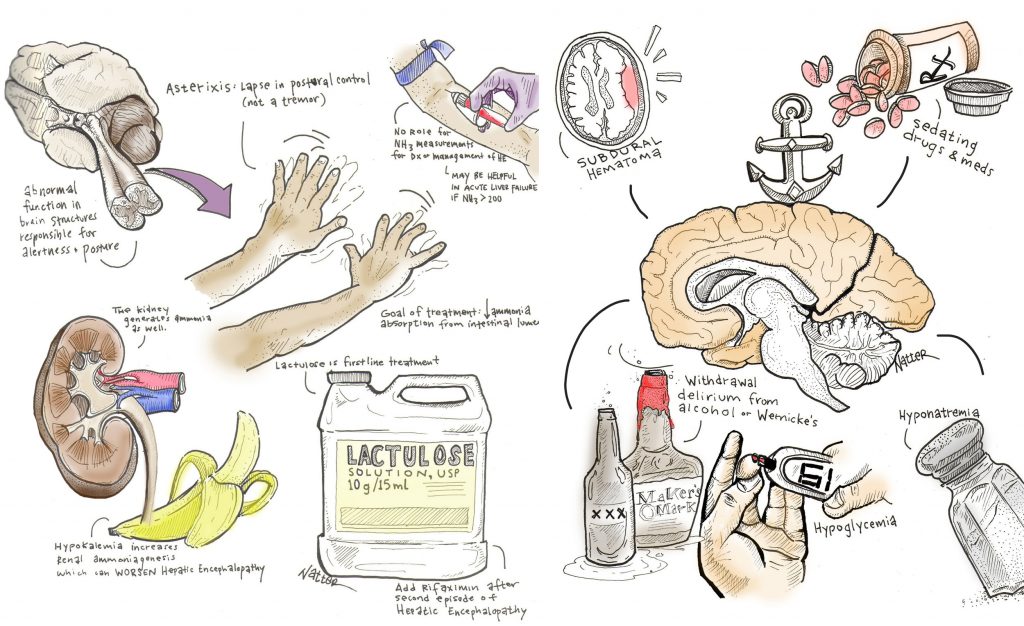
By Dr. John Hwang MD, Marty Fried MD and Shreya P. Trivedi MD; Illustration by Mike Natter MD.  Quiz yourself on the following 5 Pearls we’ll be covering on Hepatic Encephalopathy (HE):
Time Stamps
- What are other causes of altered mental status in cirrhotics? What are common precipitants for an acute episode of HE? (1:45)
- What is asterixis? What is the diagnostic utility of a cirrhotic with asterixis? (6:10)
- How do lactulose & rifaximin work? What are their indications? (11:00)
- What is the connection between hypokalemia and HE? (14:10)
- What is the discriminatory power of an ammonia level in HE? In what situation does the NH3 has stronger predictive value? (16:40)
Subscribe to CORE IM on any Podcast app! Follow us on Facebook @Core IM, Twitter @COREIMpodcast and Instagram @core.im.podcast. Please give any feedback to COREIMpodcast@gmail.com.
Shownotes
Pearl 1:
- Try not to anchor on hepatic encephalopathy in an altered cirrhotic patient. Â
- Examples of other common conditions that depress consciousness and tend to be misdiagnosed as HE include subdural hematomas, wernicke’s encephalopathy, sedating drugs and medications, withdrawal delirium from alcohol or benzodiazepines, hyponatremia, hypoglycemia, SBP, Co2 narcosis, etc.  Â
- Common precipitating factors for acute hepatic encephalopathy:Â Â
- Medication nonadherence
- Infection
- Increased generation of ammonia, such as during a GI bleed or increased azotemia from overdiuresis, volume depletion or acute renal insufficiency
- Decreased liver clearance of ammonia, such with alcoholic hepatitis, portal vein thrombosis, HCC or increased shunting after a TIPS
- Electrolytes disturbances Â
Pearl 2:
- Asterixis = lapse in postural control, not a tremor. There are many ways to check for it.Â
- Asterixis reflects an abnormal function in brain structures responsible for alertness and posture. Â
- Asterixis can be seen in any form of toxic-metabolic encephalopathy, and even in thalamic/BG lesions and NOT specific to cirrhosis.
- Asterixis is only one symptom of hepatic encephalopathy; changes in cognition, affect, personality, and arousal are equally important.
Pearl 3:
- The goal in treatment is to reduce ammonia absorption from the intestinal lumen. Â
- In addition to treating reversible causes, there are two major categories of treatments: antibiotics and disaccharides
- Lactulose is first-line for both treatment of HE and for prevention of recurrence.
- AASLD’s recommendation is to add rifaximin to lactulose after the second episode of HE (grade 1 A recommendation).Â
Pearl 4:
- The kidney also generates ammonia. Hypokalemia increases renal ammoniagenesis and can precipitate or worsen HE.
- Correcting hypokalemia in HE is essential.
Pearl 5:
- There is no role for NH3 measurements in diagnosis or management of HE.
- There might be a role in acute liver failure where an arterial NH3 >200 is associated with higher risk of cerebral edema and herniation. Â
Many thanks to Dr. Sonja Olsen for peer-reviewing this podcast!
ReferencesÂ
- Bass NM, Mullen KD, Sanyal A, et al. Rifaximin treatment in hepatic encephalopathy. The New England journal of medicine 2010;362:1071-81.
- Bustamante J, Rimola A, Ventura PJ, et al. Prognostic significance of hepatic encephalopathy in patients with cirrhosis. Journal of hepatology 1999;30:890-5.
- Clemmesen JO, Larsen FS, Kondrup J, Hansen BA, Ott P. Cerebral herniation in patients with acute liver failure is correlated with arterial ammonia concentration. Hepatology 1999;29:648-53.
- Ong JP, Aggarwal A, Krieger D, et al. Correlation between ammonia levels and the severity of hepatic encephalopathy. The American journal of medicine 2003;114:188-93.
- Tapper EB, Jiang ZG, Patwardhan VR. Refining the ammonia hypothesis: a physiology-driven approach to the treatment of hepatic encephalopathy. Mayo Clinic proceedings 2015;90:646-58.
- Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology 2014;60:715-35.
- Weiner ID, Verlander JW. Renal ammonia metabolism and transport. Comprehensive Physiology 2013;3:201-20.