Podcast: Play in new window | Download
Subscribe: RSS
 By Amy Shen Tang MD, Marty Fried MD and Shreya P. Trivedi MD; Illustration by Michelle Lo, MD & Amy Ou, MD.  Quiz yourself on the following 5 Pearls on Chronic Hepatitis B (HBV) Management
By Amy Shen Tang MD, Marty Fried MD and Shreya P. Trivedi MD; Illustration by Michelle Lo, MD & Amy Ou, MD.  Quiz yourself on the following 5 Pearls on Chronic Hepatitis B (HBV) Management
Time Stamps
- What is the focused history, physical and lab workup in a patient with chronic HBV? (1:40)
- What is the best imaging to evaluate for intermediate stages of liver fibrosis? (4:06)
- What scoring tools can you use to estimate fibrosis and what are their limitations?
- What factors do you use to assess which patients get treatment? (7:41)
- What drugs are available for HBV treatment and how do you choose? (11:18)
- Which chronic HBV patient should be screened for HCC, and how often? (14:45)
Follow us on Facebook @Core IM || Twitter @COREIMpodcast || Instagram @core.im.podcast. Subscribe to CORE IM on any podcast app! Please give any feedback at COREIMpodcast@gmail.com.
Show Notes
Pearl 1:
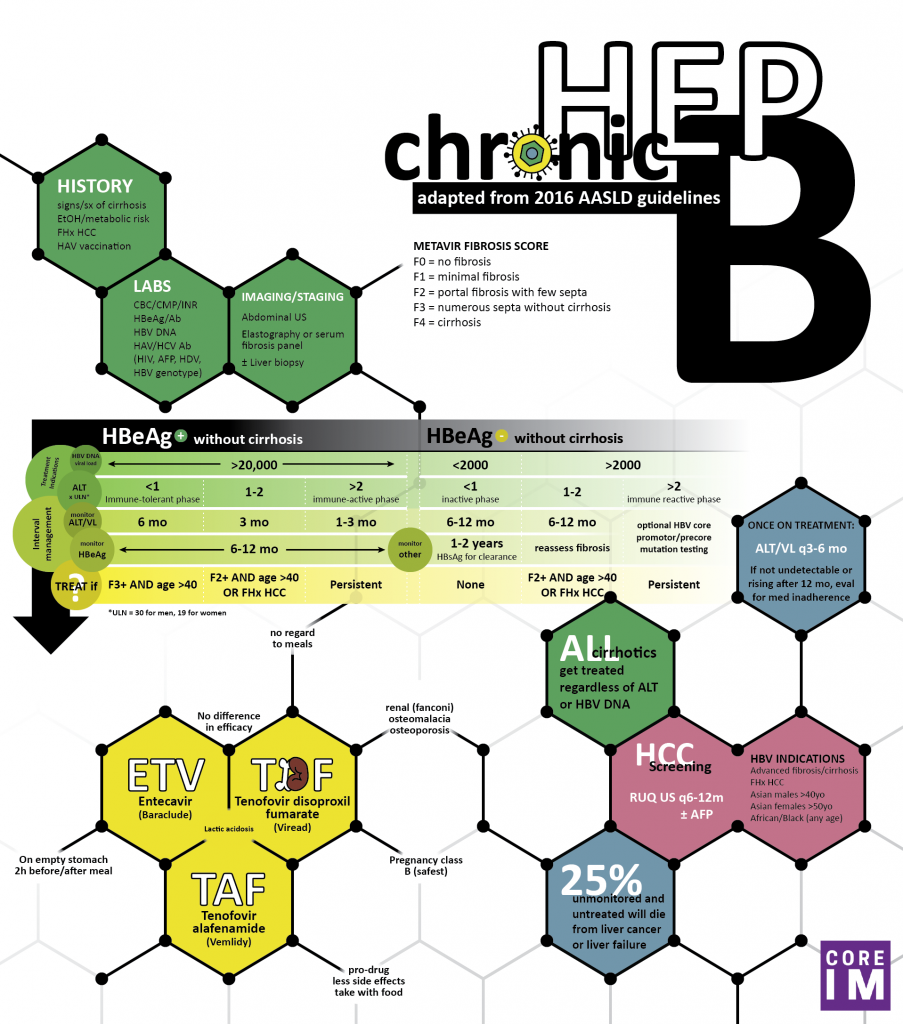
- During the initial evaluation of chronic HBV, ask about alcohol use and metabolic risk factors because alcoholic and non-alcoholic fatty liver disease is common and may contribute to fibrosis. Also, ask about family history of liver cancer as particularly virulent strains can be  transmitted vertically.
- Focus your physical exam on any signs of cirrhosis.
- Send labs markers of cirrhosis, HBV DNA level, HBeAg and anti-HBe and consider serum alpha fetoprotein (AFP)
- Regardless of whether or not these patients need to be treated, you should monitor these labs at least every 6 months because even inactive chronic HBV with low HBV DNA level and ALT can subsequently mutate, reactivate and cause problems.
Pearl 2:
- Imaging is not only important for liver cancer screening but also staging of fibrosis.
- Transient elastography (brand name Fibroscan) uses ultrasound to determine stiffness of the liver and converts its measurement into a METAVIR scoring system. It can be helpful for the fibrosis assessment, particularly in the intermediate stages. It can also help distinguish between fatty liver induced changes from that of HBV induced fibrosis
- There are a few scoring tools used to estimate fibrosis called the APRI or FIB-4 scores that use AST to platelet ratios, but will only be abnormal in advanced cirrhosis.
Pearl 3:
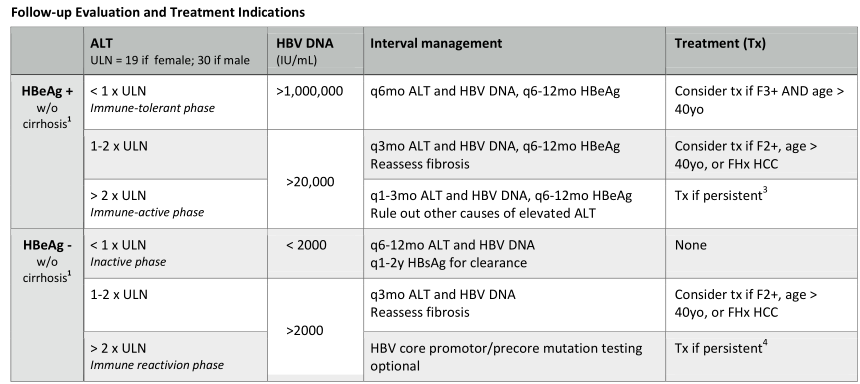
- AASLD defines the ALT upper limit of normal (ULN) as 30 for men and 19 for women. Â An ALT that is 2x the ULN, meaning ALT 60 and 38 for men and women, is an indication to treat in HBeAg positive patients and HBeAg negative patients if HBV DNA level is also elevated (> 2000 IU/mL).
- All patients with cirrhosis be treated regardless of VL or ALT.
- The key variables for treatment indication: HBeAg status first followed by VL, ALT and fibrosis. (see table)
- Other considerations for treatment include a family history of HCC Â or age > 40.
Pearl 4:
- There are 3 medications that are as first-line antiviral treatment for chronic HBV: Â entecavir and the two tenofovir drugs, Â TDF (tenofovir disoproxil fumarate, trade name Viread) and the new TAF (tenofovir alafenamide, Trade name Vemlidy). Â
- There is no significant difference in efficacy between tenofovir and entecavir Â
- TDF has some risk of kidney damage (Fanconi syndrome) and osteopenia though the risk is mitigated in the new agent, TAF. Â
- TDF (pregnancy category B) is the only option suitable for pregnant patients and can be taken WITHOUT regard to meals.
Pearl 5:
- HCC screening is based on risk factors such as family history of HCC, personal history of cirrhosis, ethnicity and sex of the patient with chronic hepatitis B.
- It starts at the time of diagnosis for African patients, age 40 for Asian men, age 50 for Asian women.  Also, all patients w/ cirrhosis or a family hx of liver cancer should get routine screening. Â
- The AASLD recommends HCC screening with liver US every 6 months with or without serum alpha fetoprotein (AFP). Â
References
- Terrault, N. A., Bzowej, N. H., Chang, K.-M., Hwang, J. P., Jonas, M. M. and Murad, M. H. (2016), AASLD guidelines for treatment of chronic hepatitis B. Hepatology, 63: 261–283. doi:10.1002/hep.28156
- Tapper, E. B. and Lok A. S. F., Use of Liver Imaging and Biopsy in Clinical Practice. Â New England Journal of Medicine 2017; 377:756
- Lampertico, Pietro et al. Â EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. Â Journal of Hepatology , Volume 67 , Issue 2 , 370 – 398.
- Bruix, J and Sherman, M (2011). Â Â Management of Hepatocellular Carcinoma: An Update. Â Hepatology, 53(3): 1020-1058