Podcast: Play in new window | Download
Subscribe: RSS
 Let’s go deeper into to why we think about diseases the way we do: Classifications for COPD through the Years! Written by Dr. Steve Liu and Dr. Carolyn Drake || Hosted by Dr. Steve Liu, Dr. Carolyn Drake & Dr. Janine Knudsen || Graphic Design by Mr. Ramon Thompson
Let’s go deeper into to why we think about diseases the way we do: Classifications for COPD through the Years! Written by Dr. Steve Liu and Dr. Carolyn Drake || Hosted by Dr. Steve Liu, Dr. Carolyn Drake & Dr. Janine Knudsen || Graphic Design by Mr. Ramon Thompson
Time Stamps
- How did prior understanding of COPD pathophysiology lead to COPD classifications in the past? (3:25)
- How is COPD diagnosed? (6:13)
- How has COPD been classified and why? (6:42)
Subscribe to CORE IM on any podcast app! Follow us on Facebook @Core IM || Twitter @COREIMpodcast || Instagram @core.im.podcast. Please give any feedback at COREIMpodcast@gmail.com.
Show Notes:
-
- Chronic Obstructive Lung Disease (COPD), is a disease of small airway inflammation defined by at FEV1/FVC ratio less than 0.70 and symptoms of chronic bronchitis and/or emphysema.
- In 1998, the U.S. National Heart, Lung, and Blood Institute and the World Health Organization helped to form the Global Initiative for Chronic Obstructive Lung Disease (GOLD). The program’s goal was “to produce recommendations for management of COPD based on the best scientific information available.â€
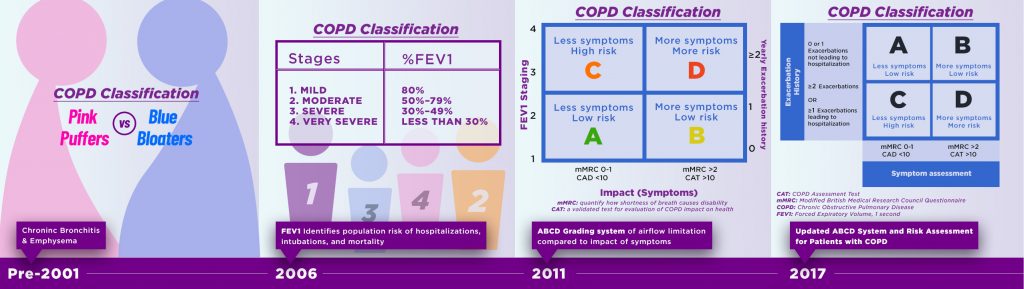
- GOLD began publishing clinical guidelines in 2001; initially they separated COPD into the clinical syndrome of “blue bloatersâ€, or chronic bronchitis, and “pink puffersâ€, or chronic emphysema, however this distinction is not used anymore.
- COPD is caused by inflammation and oxidative stress at the level of bronchioles and parenchyma. This leads to maladaptive remodeling, with dysregulation of proteinases and antiproteinases causing abnormal mucociliary function, small airways disease and alveolar loss. Actual symptoms and progression of disease vary from person to person.
- The 2006 GOLD guidelines defined COPD severity by FEV1 (forced expiratory volume in 1 second).
- FEV1 can be used to predict clinical outcomes like hospitalization and mortality on a population level, based on the placebo arms of landmark trials like TORCH, UPLIFT, and ECLIPSE.
- For example an FEV1 of <30% was associated with a 24% risk of 3-year mortality.
- However, there has been an increasing acceptance that FEV1 changes can lag behind symptoms and even imaging findings. This is based on large-scale observational studies such as COPDGene and SPIROMICS.
- As a results, the 2011 GOLD guidelines added a symptom score (using validated CAT or mMRC tools) and divided patients into groups A through D.
- Groups A and C correspond to a good functional status, whereas B and D correspond to a poor functional status (see graphic)
- However follow up studies showed that this new system using FEV1 + symptoms was not better at predicting outcomes than the FEV1-only 2001 system.
- The 2017 GOLD guidelines combined the 2006 and 2011 methods. They suggest first looking at a patient’s FEV1 to group patients into risk categories (for mortality, hospitalization, and intubations), and then using their symptom score (CAT or mMRT) and history of exacerbations to guide treatment decisions.
Many thanks to Dr. Joan Reibman, Professor of Medicine and Environmental Medicine at NYU and director of the NYU/Bellevue Asthma, Airways, and Environment Program, for peer-reviewing this episode.
References
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. 2013;187:347-65.
- Peter Lange et al. Prediction of the clinical course of chronic obstructive pulmonary disease, using the new GOLD classification. AJRCCM 2012;186(10):975-81.
- Joan B. Soriano et al. Distribution and prognostic validity of the new global initiative for chronic obstructive lung disease grading classification. Chest 2013;143(3):694-702.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of COPD. Available from: http://www.goldcopd.org
