 Sam Rougas MD
Sam Rougas MD
Faculty Peer Reviewed
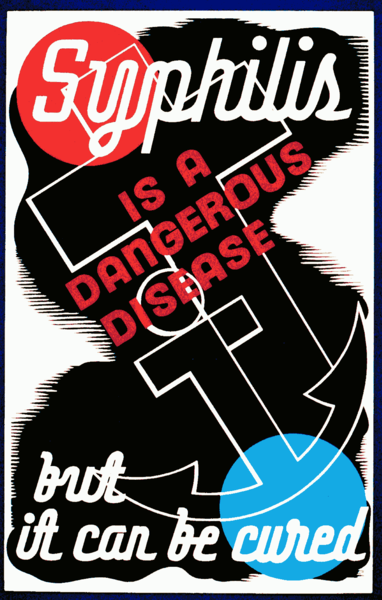
It seems that every week a new article in a major newspaper is reporting what most infectious disease physicians have been preaching for several years. Antibiotic resistance is rapidly spreading. Infections such as Methicillin Resistant Staphylococcal Aureus, Extremely Drug Resistant Tuberculosis, and Vancomycin Resistant Enterococcus have journeyed from the intensive care units to the locker rooms of the National Football League. That being said, some bacteria have strangely and until recently inexplicably behaved. Syphilis, a disease caused by the spirochete Treponema Pallidum, though first reported in Europe around the 15th century has likely been in North America since the dawn of mankind. Its rapid spread in Europe began shortly after Christopher Columbus returned from the new world[1] and remained unabated until it was first noted that Penicillin (PCN) could cure the disease[2]. However, since that time, syphilis, once the great pox, is now at the bottom of most differentials. How is it then, that one of our oldest diseases remains sensitive to our first antibiotic?Penicillin resistance to staphylococcal species was reported as early as 1946 and multiple cases were noted worldwide before the turn of the decade[3]. Literally within ten years of the existence of PCN there was resistance among staph species; however, after 50 years, PCN resistant syphilis is a worthy of a case report. In practically every case, the infection was cured with increasing the dose or duration of therapy or with another beta-lactam antibiotic[4,5]. One tempting explanation is that spirochetes are incapable of developing PCN resistance; however, that is not true. Brachyspira Pilosicoli, in intestinal spirochete has shown PCN resistance[6]. A second thought is that Syphilis is incapable of developing antibiotic resistance at all, though this too has not been shown to be true. Case reports of azithromycin resistance in T. Pallidum became increasingly common at the beginning of this century. Gene sequencing of these species mapped out the mutation leading to the macrolide resistant phenotype[7]. Obviously the mechanism of action of a macrolide antibiotic is different from a beta lactam as is the resistance profile. However, it does show that syphilis is capable of developing resistance to at least one class of antibiotic.
The classic teaching is that beta lactam antibiotics function at the level of the cell wall via binding to penicillin binding proteins (PBPs). Once bound, the beta lactams are able to interfere with the production of specific peptidoglycans critical for cell wall structure. Once these peptides are eliminated the cell wall ruptures and the bacteria dies. Resistance occurs when bacteria either via an innate mutation or via DNA exchange acquire the ability to produce beta lactamase, an enzyme cabable of cleaving the antibiotic rendering it useless. In syphilis the mechanism of action is thought to be the same, but resistance has never developed. This may be a direct consequence of one of the more recently discovered PBPs called Tp47[8]. Tp47 functions as both a PBP and a beta lactamase. However, it may paradoxically be responsible for the persistence of PCN sensitivity in syphilis. The binding of the beta lactam component of PCN to Tp47 results in hydrolysis of the beta-lactam bond of the antibiotic. However, in the process of this reaction several byproducts are created. The thought is that these byproducts have a higher affinity for Tp47 than the beta lactam itself[9]. Thus as a consequence of PCN being broken down, products are released which make it more difficult for the beta-lactamase to bind the antibiotic.
While this is one current theory behind the exquisite sensitivity of syphilis to PCN, it is clearly not cause for celebration. Cases of syphilis are increasing world-wide10 as the medical community has been unable to eradicate this disease. As the number of cases increase, so too does the potential for antibiotic resistance. Theoretically a mutation in Tp47 may alter the protective byproducts upon which the sensitivity of syphilis to PCN depends. Such a mutation would likely result in the end of the gravy train that has been the treatment of syphilis.
Â
1. Rose M. Origins of Syphilis. Archeology 1997; Volume 50 Number 1
2. Mahoney J, Arnold R, Harris A. Penicillin treatment of early syphilis; a preliminary report. Vener Dis Inform 1943; 24:355-357
3. Shanson DC, Review Article: Antibiotic-resistant staphylococcus aureus. Journal of Hospital Infection (1981) 2: 11-36
4. Cnossen W, Niekus H, Nielsen et al. Ceftriaxone treatment of penicillin resistant neurosyphilis in alcoholic patients. J. Neurol. Neurosurg. Psychiatry 1995; 59; 194-195
5. Stockli H, Current aspects of neurosyphilis: therapy resistant cases with high-dosage penicillin? Schweiz Rundsch Med Prax. 1992 Dec 1; 81(49):1473-80
6. Mortimer-Jones S, Phillips N, Ram Naresh T et al. Penicllin resistance in the intestinal spirochaete Brachyspira pilosicoli associated with OXA-136 and OXA-137, two new variants of the class D Beta-Lacatmase OXA-63. Journal of Medical Microbiology 2006; 57 1122-1128
7. Katz K, Klausner J. Current Opinion in Infectious Disease 2008, 21:83-91
8. Deka R, Machius M, Norgard M et al. Crystal Structure of the 47-kDa Lipoprotein of Treponemal Pallidum Reveals a Novel Pencillin-Binding Protein. The Journal of Biological Chemistry 2002. 277:44: 41857-41864
9. Cha J, Ishiwata A, Mobashery S. A Novel B-Lactamase Activity from a Penicllin-binding Protein of Treponema pallidum and Why Syphilis Is Still Treatable With Penicllin. The Journal of Biological Chemistry 2004. 279: 15: 14917-14921
10. Gerbose A, Rawley J, Heymann D, et al. Global prevalence and incidence estimates of selected curable STDs. Sex Transm Infections 1998; 74: 512-516
Faculty Peer Reviewed with commentary by Meagan O’brien MD, NYU Division of Infectious Diseases and ImmunologyÂ
While it is true that Treponema Pallidum remains highly susceptible to Penicillin and has developed resistance to Azithromycin through an A–>G mutation at position 2058 of the 23S rRNA gene of T. pallidum, which confers resistance by precluding macrolide binding to the bacterial 50S ribosomal subunit, of which 23S rRNA is a structural component, the mechanisms of retained Penicillin sensitivity are not fully understood[7]. The discovery of Tp47 as a dual PBP and Beta-lactamase is interesting and important, but more studies would be needed to attribute this mechanism to the persistence of Treponema Pallidum sensitivity to Penicillin. Luckily, we do not have many clinical isolates to test this theorized mechanism. One key clinical point to remember is that eradication of the infection depends not only on the invading organism, but also upon the host defense system. In our HIV+ immunocompromized patient population, we routinely are concerned about treatment failure in syphilis infection due not to penicillin drug resistance but to dysfunctional host responses. A body of evidence now exists supporting the recommendation that if an HIV+ patient has a CD4 T-cell count ≤350 cell/uL and a blood RPR titer ≥ 1:32 with latent syphilis or syphilis of unknown duration, a lumbar puncture should be performed to rule out neurosyphilis, and if positive, that intravenous penicillin should be given instead of IM Benzathine Penicillin[11-14]. Additionally, after treating late or latent syphilis, a fall in RPR titer by 1:4 needs to be observed over 12 months or the patient should be evaluated for treatment failure or neurosyphilis, with the understanding that the CNS may be a more privelidged site for Treponema survival in the face of IM Benzathine Pencillin.
11. Marra, C.M., C.L. Maxwell, S.L. Smith, et al., Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis, 2004. 189(3): p. 369-76.
12. Marra, C.M., C.L. Maxwell, L. Tantalo, et al., Normalization of cerebrospinal fluid abnormalities after neurosyphilis therapy: does HIV status matter? Clin Infect Dis, 2004. 38(7): p. 1001-6.
13. Ghanem KG, Moore RD, Rompalo AM, Erbelding EJ, Zenilman JM, Gebo KA. Lumbar puncture in HIV-infected patients with syphilis and no neurologic symptoms.
Clin Infect Dis. 2009 Mar 15;48(6):816-21.
14. Ghanem KG, Moore RD, Rompalo AM, Erbelding EJ, Zenilman JM, Gebo KA. Neurosyphilis in a clinical cohort of HIV-1-infected patients. AIDS. 2008 Jun 19;22(10):1145-51.

4 comments on “Why is Syphilis Still Sensitive to Penicillin?”
Very interesting…
Well, this is supposed to be how antibiotics work, by punching a hole in the cell wall of the bacteria. Caprillic acid in coconut oil does the same thing. But why theorized? With the current technology, this supposed action of Treponema destruction should be able to be viewed in real time, If the researchers are only looking for resistance via beta lactamase production, and not the dna alteration into a different gene, they would see exactly what they do see, no resistance. It seems to me that penicillin is a product, being derived from bread mold, that would have been contemporaneous with this human bacteria.
In order to claim a cure would not he evidence be a real-time video capture of the bacteria’s supposed death? Not just its absence of beta lactamase production.
Comments are closed.