Podcast: Play in new window | Download
Subscribe: RSS
 By Daniel Sartori MD, Marty Fried MD, Shreya Trivedi MD; Illustration by Michelle Lo MD and Amy Ou MD. Quiz yourself on the 5 Pearls we will be covering:
By Daniel Sartori MD, Marty Fried MD, Shreya Trivedi MD; Illustration by Michelle Lo MD and Amy Ou MD. Quiz yourself on the 5 Pearls we will be covering:
- What are signs and symptoms of chronic adrenal insufficiency (AI)? What is the most sensitive? (2:02)
- How do we diagnose and differentiate types of adrenal insufficiency? (6:05)
- How sensitive and specific are the diagnostic tests for AI Â and at what cutoffs? (12:06)
- Can we both test and treat adrenal insufficiency at the same time? (16:40)
- Throwback: How do hypokalemia and hepatic encephalopathy connected? (24:55)
- Dr. Nidhi Agrawal Recap (19:20)
A special thank you to Dr. Nidhi Agrawal for peer-reviewing this podcast!
Subscribe to CORE IM on any podcast app! Follow us on Facebook @Core IM || Twitter @COREIMpodcast || Instagram @core.im.podcast. Please give any feedback at COREIMpodcast@gmail.com.
Pearl 1
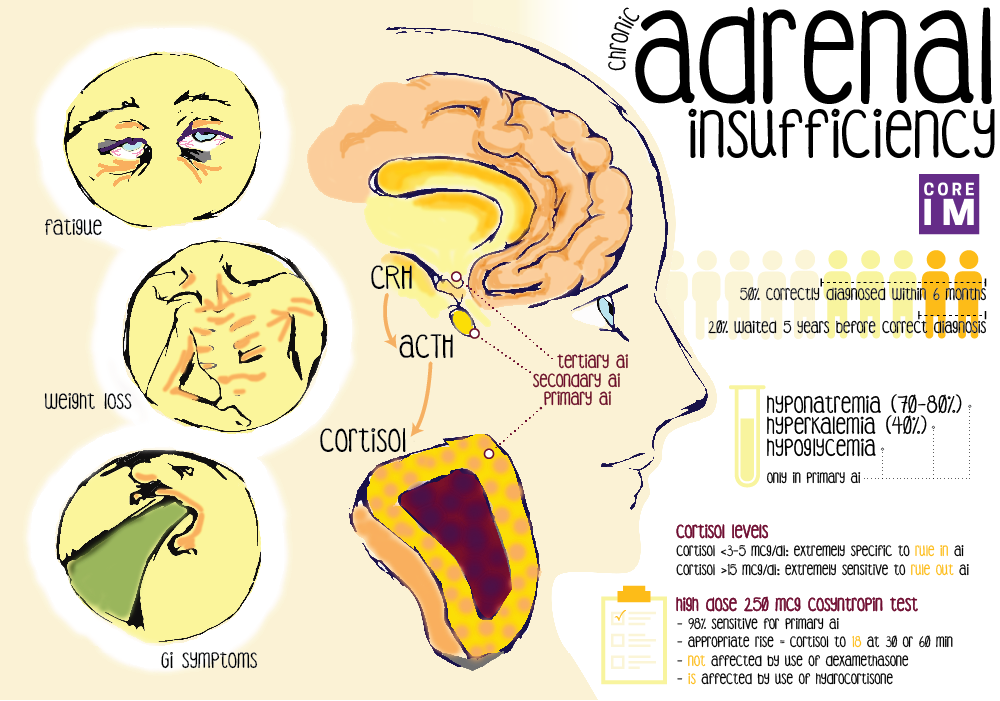
- Signs and symptoms of adrenal insufficiency are often very vague and non-specific.
- Symptoms:Â fatigue (most sensitive symptom), weight loss, GI complaints, psychiatric complaints.
- Exam: Hypotension and/or orthostasis. Hyperpigmentation, especially over hands and knuckles, is specific, but this is exclusively seen in primary  AI.
- Labs: Â
- Most lab abnormalities are due to mineralocorticoid deficiency and these are seen in primary AI only. These include hyponatremia, hyperkalemia, hypoglycemia.
- Eosinophilia, while commonly taught, is in fact largely theoretical and occurs rarely with AI.
Pearl 2
- The diagnosis and localization of the defect can be determined by: AM serum cortisol, serum ACTH level, response of serum cortisol to ACTH-stimulation (the cort stim test)
- Possibilities of various tests results and diagnosis:
- High ACTH, low AM serum cortisol, low serum cortisol after stimulation
- Diagnostic for primary AI.
- Low ACTH, low AM cortisol, normal cortisol after stimulation
- Diagnostic of either secondary or tertiary AI. Â The adrenals can be stimulated appropriately and will respond by pumping out cortisol
- Low ACTH, low AM cortisol, low cortisol after stimulation
- Diagnostic of either secondary or tertiary but indicates long standing AI. There is likely adrenal atrophy because the adrenals are not responding to cortisol stimulation.
- High ACTH, low AM serum cortisol, low serum cortisol after stimulation
- In secondary or tertiary AI, patients should still have a normal renin-angiotensin-aldosterone system (RAAS) but a patient with a PRIMARY adrenal lesion may not.
- In primary AI, the lesion is at the level of the adrenal cortex itself and there can be ‘collateral damage’ to other layers, like the layer that secretes aldosterone.
Pearl 3
- AM Cortisol:
- At this threshold 3-5mcg/dL, AM cortisol is an extremely specific, and can rule in adrenal insufficiency.
- At this threshold 15mcg/dL, AM cortisol is an extremely sensitive and can rule out adrenal insufficiency. Â This value or above successfully predicts normal adrenal function
- Cort Stim Test:
- High dose test (250mcg consyntropin) is the standard and has 98% sensitivity for primary adrenal insufficiency. Â
- A normal high dose stim result can almost certainly rule out adrenal insufficiency.
- A normal high dose stim results is defined as a rise in serum cortisol to 18mcg/dL at either 30 minutes or 60 minutes after stimulation
- Cortisol levels are episodic, vary throughout the day so timing matters – measuring cortisol levels in the morning improves the test’s specificity.
- Cortisol circulates bound to cortisol binding globulin (CBG) and albumin so conditions that affect levels of these proteins will give the impression that cortisol levels are either high or low independent of the actual free hormone concentration.
Pearl 4
- Almost all steroids cross react with assays for serum cortisol with the exception of dexamethasone
- If treatment is already given, the cort stim test (not AM cortisol) can be helpful, as the exogenous steroids will invariably suppress the AM cortisol.
- Options for treatment and still testing if the HPA axis is intact (cort-stim test)
- Use dexamethasone (this will not cross react with our assay)
- Use hydrocortisone and hold the dose prior to testing
Pearl 5
- The kidney generates ammonia. Hypokalemia increases renal ammoniagenesis and can precipitate or worsen hepatic encephalopathy (HE).
- Correcting hypokalemia in HE is essential.
References
Irvine, W. J., and E. W. Barnes. “Adrenocortical insufficiency.” Clinics in Endocrinology and metabolism. 1.2 (1972): 549-594.
Bancos, Irina, et al. “Diagnosis and management of adrenal insufficiency.” The Lancet Diabetes & endocrinology 3.3 (2015): 216-226.
Bornstein, Stefan R., et al. “Diagnosis and treatment of primary adrenal insufficiency: an endocrine society clinical practice guideline.” The Journal of Clinical Endocrinology & Metabolism 101.2 (2016): 364-389.
(2:33) Bleicken B, Hahner S, Ventz M, Quinkler M. Delayed diagnosis of adrenal insufficiency is common: a cross-sectional study in 216 patients. Am J Med Sci. 2010;339(6):525.
(4:58) Spry C. Eosinophilia in Addison’s disease. Yale J Biol Med. 1976;49(4):411.
(12:33) Erturk E, Jaffe CA, Barkan AL Â Evaluation of the integrity of the hypothalamic-pituitary-adrenal axis by insulin hypoglycemia test.. J Clin Endocrinol Metab. 1998;83(7):2350.
(12:55) Galbois A, Rudler M, Massard J, Fulla Y, Bennani A, Bonnefont-Rousselot D, Thibault V, Reignier S, Bourrier A, Poynard T, Thabut D. Â Assessment of adrenal function in cirrhotic patients: salivary cortisol should be preferred. J Hepatol. 2010;52(6):839. Epub 2010 Mar 15.
(13:31) Cartaya, Julia, and Madhusmita Misra. “The low-dose acth stimulation test: is 30 minutes long enough?.” Endocrine Practice 21.5 (2015): 508-513.
