Podcast: Play in new window | Download
Subscribe: RSS
 Join us in this episode as we question everything you ever thought you knew about… acetaminophen and fevers || By Steven R. Liu MD and Dr. Janine Knudsen MD || Graphic Design by Ramon Thompson
Join us in this episode as we question everything you ever thought you knew about… acetaminophen and fevers || By Steven R. Liu MD and Dr. Janine Knudsen MD || Graphic Design by Ramon Thompson
Time Stamps:
- What data is there to support the use of acetaminophen as a fever reducer? (2:08)
- Does acetaminophen improve patient outcomes? (4:30)
- How does acetaminophen compare to other medications like NSAIDs? (9:56)
- What is the mechanism of acetaminophen action? (10:50)
- Review of teaching points (16:02)
Thank you to Dr. Michael Pillinger, Professor of Rheumatology at NYU and Chief of Rheumatology at the NY Harbor VA Hospital, for peer reviewing this podcast!
Subscribe to CORE IM on any podcast app! Follow us on Facebook @Core IM || Twitter @COREIMpodcast || Instagram @core.im.podcast. Please give any feedback at COREIMpodcast@gmail.com.
Show Notes:
- How effective is acetaminophen? Studies show that the effect is moderate studies show that it only reduces fevers by 0.0 to 0.3 degrees centigrade on average, while others showed that patients hospitalized with infection who received acetaminophen defervesced slightly faster than patients who got placebo.
- Does acetaminophen improve hospital outcomes? An observational study of critically ill patients with infection found that in-hospital and ICU mortality decreased in patients who received acetaminophen.
- However their control group had significant differences, raising concern for confounding. Also when they honed in on medical patients only (excluding surgical ICU patients), the differences between cases and controls became less impressive.
- Does promoting euthermia improve outcomes in infection? Â Both small and large RCTs of ICU patients who were cooled with both acetaminophen and ice did not show significant improvements in long-term mortality.
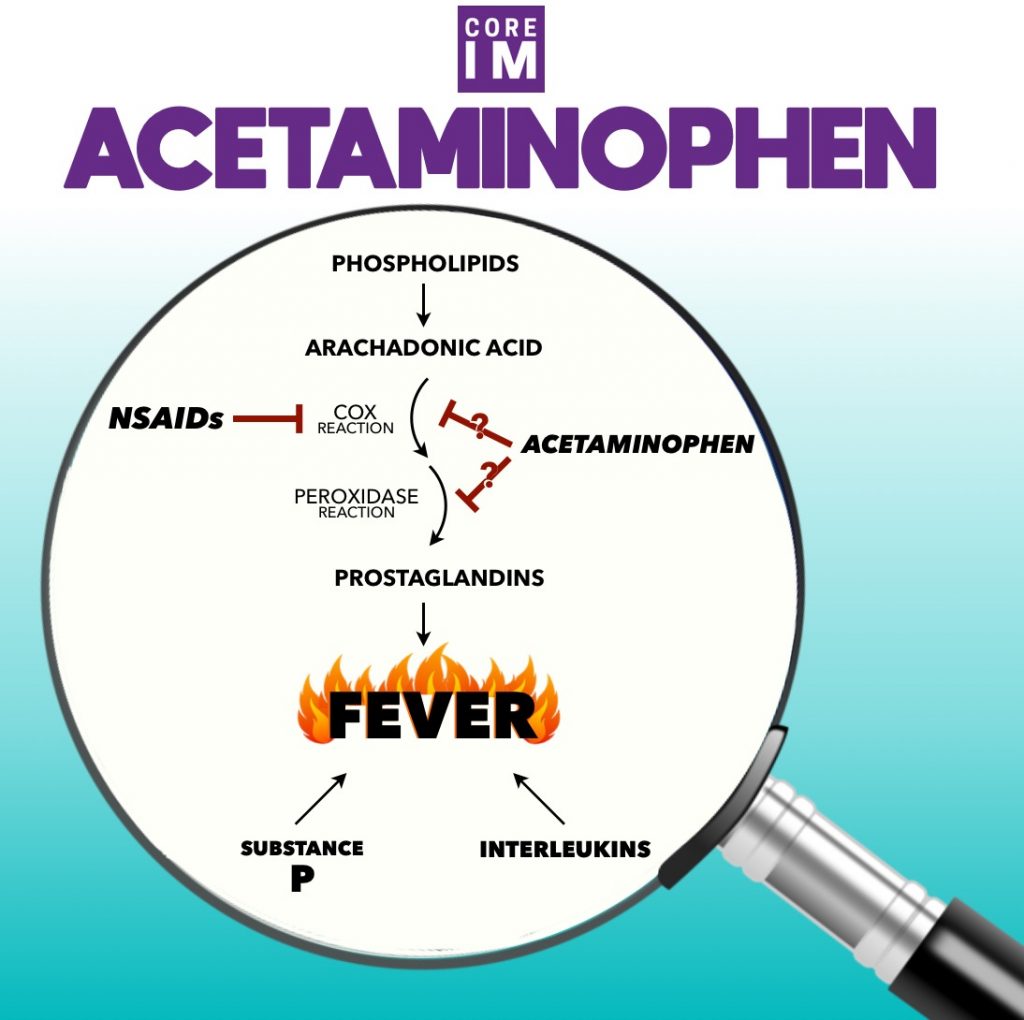
- How does acetaminophen work compared to NSAIDs? Â Both likely inhibit COX from making prostaglandin E, which works in the hypothalamus to stimulate fevers. However NSAIDs also block COX in the periphery to reduce inflammation, whereas acetaminophen is less effective in the periphery so is not a good anti-inflammatory medication.
- Does acetaminophen work differently than NSAIDs? Some studies suggest that acetaminophen blocks the peroxidase step of COX, which blocks prostaglandin production in the brain, but does not lower it much in the periphery. But the jury is still out on its definitive mechanism.
Transcript:
S: So, when I was growing up TV shows like Goosebumps or Twin Peaks about creepy things in seemingly quiet towns were hitting a new stride.
J: My personal favorite was “are you afraid of the dark?â€
S: Oh what a classic. Yeah so to be special we’d tell our own creepy stories. But, I remember hearing that our town for real was the site of a series of murders that led to the introduction of tamper-safe seals on medications.
J: Whoa. That’s pretty grim. I thought it was an urban legend until I read more about it.
S: Yeah, I’m not sure I would have believed it myself.
J: And so we checked it out on wikipedia
S: Where else?
J: And found an old news article that told the story of the murder of seven people in Chicago from Tylenol laced with cyanide.
S: They never did find the culprit, but suspects ranged from an extortionist in New York City to apparently even the Unabomber.
J: It of course made national headlines, and in response, Congress passed a federal law requiring all over the counter medications to have tamper-proof seals.
S: But this wasn’t just some random over the counter med! It was Tylenol, the number one selling medication in the US at the time.
J: And even decades later, it’s still a go-to medication for a fever when you’re in hospital.
S: Or even yourself when you’re stuck at home with the flu.
J: So today we’re going to be talking about, first, what data there is to support the use of acetaminophen as a fever reducer.
S: And how does it compare to other fever reducers like NSAIDs?
J: And for something we so frequently put into our bodies, how does it really even work?
S: Spoiler alert, we’re still not really sure, but exploring this will take us down the winding road of complicated pathophysiology
J: That has plenty of dead ends
S: But may finally end with hopefully a satisfying discussion about why we think about it
J: And use it
S: The way we do.
J: So let’s jump into the world of acetaminophen, a drug we all use, but hardly know.
[INTRO]
J: So let’s start by reviewing what evidence we have to guide us
S: Or justify…
J: Our ordering Tylenol at the first sight of a fever.
S: So sometimes basic numbers are the easiest. How much does acetaminophen really lower fevers?
J: On average, numbers tend to range between three tenths of a degree centigrade to no change in terms of fever reduction.
S: And that’s about half a degree Fahrenheit.
Jefferies S, et al. “Randomized controlled trial of the effect of regular paracetamol on influenza infection.†Respirology (2016) 21, 470-477.[LS2]
Young P, et al. “Acetaminophen for fever in critically ill patients with suspected infectin.†NEJM Dec 3 2015.
Greenberg RS, Chen H, Hasday JD. “Acetaminophen has limited antipyretic activity in criticall ill patients.†J Crit Care. 2010 June ; 25(2): 363e1-363e7.
J: Thanks… But that can be a bit deceptive because what we’re talking about here is average temperatures.
S: And to a degree
J: Terrible pun
S: I liked it. But to a degree, it makes sense that averages don’t change that drastically. After all, even if acetaminophen suppresses fevers, it’s not curing an infection. So you’re still likely to get more fevers.
J: This idea is similar to using beta-blockers to improve sinus tach. Sure it will probably slow down a heart rate, but we’re not gonna just stick our heads in the sand and pretend that beta-blockers are a first line treatment for sinus tach.
S: In other words, it might make your fever go down, but if it comes back, you may not see a huge benefit when we look at average 24 hour temperatures.
J: So why are we so confident that it works?
S: Well ideally, you’d probably want a trial that looks more at its effects in the short term?
J: And we have exactly that. There’s a nice randomized controlled trial from last year called “Randomized, controlled, multicentre clinical trial of the antipyretic effect of intravenous paracetamol in patients admitted to hospital with infectionâ€. It looked specifically at this.
Tsaganos et al. “ibid†Br J Clin Pharacol. 2017 Apr;83(4)742-750.
S: I quickly wanna highlight that this was using intravenous acetaminophen
J: Grumble grumble (yeah we don’t have to include this)
S: And it was a fairly small 80 person trial, but otherwise it’s pretty applicable.
J: They looked at people over the age of 18, with new fevers over 38.5 degC
S: That’s 101.3 deg F
J: And with either skin, urinary, or upper respiratory tract infections.
S: People either got APAP or placebo in a randomized and blinded fashion. What they found was that at 6 hours, temperatures decreased by about half a degree centigrade
J: That’s about 1 degree Fahrenheit.
S: Hey that’s my line.
J: And as a quick check we realize 1 degree is more than the previous papers we mentioned, but it only looked at 6 hour window rather than the 24 hours in the other studies.
S: And they also found that median time to defervescence dropped from 6 hours to 3 hours with acetaminophen.
J: Another way to see this is that 80% of the patients getting APAP deferevesced by 6 hours compared to only 40% in the placebo group.
S: So as you might expect this led to the placebo group having a higher number of patients that would require “rescue†dosing or guaranteed APAP administration by 6 hours.
J: Well even with this modest efficacy on temperatures, does giving acetaminophen seem to help with hospital outcomes?
S: So there are a number of articles that suggest it could
J: Back in early 2015, one group published the “Paracetamol therapy and outcome of critically ill patients: a multicenter retrospective observational study.â€
Suzuki S et al. “Paracetamol therapy and outcome of crticially ill patients: a multicenter retrospective observational study.†Critical Care (2015) 19:162.
S: The name at least tells you what they were trying to accomplish. Not surprisingly, this was a large study, totaling over 15000 ICU patients.
J: Prior meta-analyses had suggested that acetaminophen was not actually associated with a reduction in-hospital mortality for critically ill patients. So they designed this observational study to see if it was worth creating an RCT to re-evaluate this question.
S: Their hypothesis was that acetaminophen probably doesn’t help critically ill patients generally, but that in patients with infection specifically, administration of acetaminophen might be associated with changes in the risk of death.
J: They found that there was an overall unadjusted reduction from 20% to 10% for in hospital mortality, and a reduction from 14.9% to 5.3% mortality in ICU patients.
S: That being said, this was not an RCT, so take that info with a grain of salt! Like most observational studies, their Table 1 suggested that the two groups were very different so over extrapolate this at your peril.
J: Still, with multivariate logistic regression analysis, they still found that receiving acetaminophen significantly reduced in-hospital mortality with an adjusted odds ratio of 0.6.
S: Interestingly, when discounting surgical patients-
J: Who might more often be receiving acetaminophen as an analgesic rather than an anti-pyretic-
S: Medical patients with fevers and infection no longer showed this increased survival. It did delay death though.
J: Wait, so all those fevers I got rid of as an overnight intern by handing out acetaminophen like candy… didn’t actually help? I thought euthermia was a really important thing in patients with infection?
S: Yeah, basically, this study we just talked about says no…
J: But what about septic shock? I thought that we now focus on euthermia.
S: They did study this. There’s a small RCT published in 2012 called “Fever control using external cooling in septic shock, a randomized controlled trial†that looked at this question with about 200 patients. Note they did not focus on their use of acetaminophen.
Schortgen F. “Fever control using external cooling in septic shock, a randomized controlled trial†Am J Respir Crit Care Med 2012 185:10:1088-1095.
J: They found that cooling decreased vasopressor requirements and improved early mortality rates (at 14 days).
S: But that it again didn’t change mortality rates by the time of discharge, again showing this effect of delaying death but not actually preventing it.
J: So with that study and other trials there was enough interesting background data circulating to set up a proper randomized control trial to answer this question – if there was any mortality or any other benefit to using acetaminophen in the ICU.
S: Enter the cleverly named HEAT trial whose title in no way spells heat.
J: This trial Acetaminophen for Fever in Critically Ill Patients with Suspected Infection
was a prospective, blinded randomized control trial geared at looking at the highest risk patients in the hospital
S: ICU patients
J: To see if there was an improvement in ICU-free days with acetaminophen
S: And it is probably one of the larger acetaminophen trials to date, coming in at exactly 700 patients in total. The people in the intervention group got 1 gram of intravenous acetaminophen every 6 hours.
J: And what they found was that there were no changes in their primary outcome between the two groups with number of ICU-free days at day 28. Nor did they see a change in probability of survival at 90 days between using acetaminophen and placebo.
S: They did briefly see a short lived improvement in survival that quickly faded by day 30.
J: Yeah – the same thing that happened in the observational trial. Acetaminophen delayed death, but didn’t ultimately prevent it.
S: They did look into that further with a sub group analysis. And it showed that patients who ultimately survived were more likely to get out of the ICU sooner if they got acetaminophen.
J: But among patients who ultimately passed away, they lived longer… but in the ICU.
S: So averaging those two outcomes together, it looked like patients who received acetaminophen had the same number of ICU days as those in the placebo arm.
J: So ultimately and not at all surprisingly, the authors note that further investigation is probably warranted.
S: One thing to remember with these trials is that we’re talking about mortality, but based on what we know about sepsis, fevers and fever control aren’t really thought to affect that.
J: Fevers are really more of a marker of infection, not mortality. Fever control may signal instead how attentive the medical team is to their patient. So to bring this all back, this data does call into question whether or not we should be giving antipyretics at all.
S: But it does highlight at least what’s become a common theme in our discussions; that focusing on numbers doesn’t always translate to better patient care.
J: So what do you do Steve?
S: I still give it. I think part of me thinks that it’s relatively a low risk medication in this context of fever reduction, so if it’ll make them feel better why not help a patient out. After all more than one patient has honestly actively asked me “why not give me tylenol? If I wasn’t here I could just buy the stuff myself.â€
J: Yeah, I agree, as long as I stay below the recommended daily dose of 3g, I give acetaminophen to my patients to help them feel better.
S: So we agree, but the next question might be – do you need to be giving acetaminophen.
J: As opposed to what?
S: No NSAIDs! There is a significant body of literature in the pediatrics data suggesting that in fact NSAIDs might be superior to APAP when it comes to fever reduction
Narayan, Kaajal, et al. “Effectiveness of paracetamol versus ibuprofen administration in febrile children: A systematic literature review.” Journal of paediatrics and child health 53.8 (2017): 800-807.
Hay, A. D., et al. “Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial.” Health Technol Assess 13.27 (2009): 1-163.
J: And even more data suggests that maybe alternating between the two is superior to any one alone.
S: I guess in terms of the applicability to adult medicine it comes down to whether or not you think that kids are really just little big people.
J: Or in your case, maybe just an overgrown little person!
S: I opened myself up for that.
J: But after all, we’re going to hopefully avoid insulting the entire field of pediatrics by recognizing that pediatric diseases and adult disease aren’t the same for many reasons.
S: And it’s not clear you can extrapolate from one group to the next.
J: And so let’s stick to what we do know. One of those things is how NSAIDs actually work.
S: To reorient you guys, we’re leaving the realm of evidence based medicine and we’re gonna talk about NSAIDs, APAP, COX, and fever pathways.
J: The purpose of this is to highlight both how we think APAP might work, and how that plays a role in how we think about using it. So for those of you not interested in this pathophys, feel free to skip to the end.
S: To recap, NSAIDs act on inhibition of an enzyme called cyclooxygenase or COX.
J: As a brief refresher for you guys, COX comes in two known isoforms, COX-1 and COX-2. And it allows for conversion of arachadonic acid to prostanoids like prostaglandin or thromboxane.
S: These prostanoids, most specifically prostaglandin E, have been known to have a role in generating fevers by their action in thermoregulatory regions of the hypothalamus.
J: Yeah we found Early experiments showed that direct injection of prostaglandin E into the hypothalamus would generate fevers.
S: Wow that sounds pretty brutal.
J: They further confirmed this physiology of fevers with an experiment that showed that COX-2 not COX-1 is responsible for making prostaglandin E in the hypothalamus. They did this by working with COX knockout mice.
S: Not to be confused with Mike Tyson Punch-Out mice. Just a little 80s era joke for you.
J: Yeah I think they get it. So the experiments with knockout mice suggested that pyrogens, or fever producers, didn’t generate fevers in COX-2 knockout, meaning that COX-2 was probably necessary for a fever to happen.
S: But that said, we don’t want to oversimplify things by pretending all fevers are due to prostaglandin E
J: There is a figurative bowl of alphabet soup
S: Things like substance P and interleukins
J: That also plays a huge role in fever generation and the complex system of thermoregulation. A lot of which is still debated and discussed.
Zampronio AR, Soares DM, Souza GEP “Central mediators involved in the febrile response: effects of antipyretic drugs†Temperature 2:4, 506-521; Oct/Nov/Dec 2015.)
Prajitha N, Athira SS, Mohanan PV “Pyrogens, a polypeptide produces fever by metabolic changes in the hypothalamus: Mechanisms and detections†Immunology Letters Vol 204, December 2018, 38-46.
S: But this knowledge is hard to ignore, especially since NSAIDs suppression of prostglandin E production probably plays a role in their ability to suppress fever.
J: And so what about APAP? Is that how it works too?
S: This has been a source of debate for some time, and the truth is that while we’re not really sure even as early as the 1970s, we’ve thought that APAP works in the brain and not elsewhere.
Vane JR, Flower RJ “Inibition of prostaglandin synthetase in brain explains the anti-pyretic activity of paracetamol.†Nature. 1972:240:410-411.
J: Sometimes it’s easier to use contrasts to understand a topic better. so to help you understand why we think that, let’s look at the clinical difference in when we use NSAIDs vs. APAP.
J: NSAIDs can treat fever – they inhibit COX function and reduce prostaglandin as a result, so the hypothalamus doesn’t trigger a fever. And clearly NSAIDs affect both the CNS and the body in general since they act as anti-inflammatories in the periphery.
S: But let’s contrast that with acetaminophen. Similar to NSAIDs it seems to have good central nervous system effects, as a pain and fever reliever. But, conversely, we don’t use it for an anti-inflammatory effects suggesting that they don’t affect the periphery.
J: So the theory is that acetaminophen probably targets something in the brain and only the brain
S: And that something could be COX-2… at least given the knockout mice data we alluded to earlier – at least that’s what the leading theory has been since the 70s.
Vane JR, Flower RJ “Inhibition of prostaglandin synthetase in brain explains the anti-pyretic activity of paracetamol.†Nature. 1972:240:410-411.
J: Ok – so final takeaway?
S: The thought is that both NSAIDs and acetaminophen act on central cox-2 explaining why they can control fever.
J: So then how does acetaminophen get comparable levels of anti-pyretic effects? Is it really more active in the brain?
S: So what do we think now?
J: Well it’s still complicated but nowadays people think that actemainophen probably works on some other pathway, or if it does act on COX, it acts on its lesser known peroxidase step.
S: COX has two steps, one is its namesake, the cox-step, the other is the peroxidase step.
J: We’ll try not to get bogged down in the details of it all, but basically some people think that APAP might work on the second peroxidase step.
S: As its name implies, the second step, peroxidase, interacts with peroxide.
J: But, if you have a bunch of peroxide around, APAP isn’t able to stop all of it from interacting with COX
S: Which limits how effective APAP is in tissue with lots of peroxide.
J: And this might explain why it is less active in some tissues than others
S: Peroxide levels are probably higher in areas of active inflammation
J: You may remember that white blood cells can make free radicals
S: A byproduct of this “superoxide” reaction is peroxide.
J: So this might explain why we observe that acetaminophen can act as a fever reducer in the hypothalamus, but not an anti-inflammatory in the periphery where peroxide levels are high.
S: But again, a lot of this is to explain what we already think we know that acetaminophen is not a great anti-inflammatory
J: Other hypotheses also exist suggesting acetaminophen and NSAIDs may both influence other fever pathways independent COX and prostaglandin.
S: Fun kind of real world fact, if you ever get stung by the Brazilian yellow scorpion, you’ll get a fever.
J: Where are you going with this?
S: But this is one of those fevers that isn’t related to prostaglandin. And wouldn’t you know, acetaminophen still works there as an antipyretic.
J: Apologies to any Brazilian listeners. But I’m not sure that remotely constitutes a “real world fact.â€
S: I just thought I would try to make things a little more applicable again.
J: Ok, so let’s do that by actually recapping things. So to start, 1) APAP may modestly decrease average fevers.
S: That effect may be more apparent in the short term with faster and more robust defervescence even if it doesn’t play out in the long term.
J: There probably isn’t good data to suggest that acetaminophen improves mortality
S: But that doesn’t mean it’s not a worthwhile drug for treatment of symptoms.
J: That’s up to you to decide for yourself, just like 3) maybe there’s data to support the use of NSAIDs over APAP.
S: And 4) in order to treat Brazilian yellow scorpion stings, use APAP.
J: Because sometimes you don’t have to know why something works, real world experience is good enough.
References:
- Markel, Howard. How the Tylenol murders of 1982 changed the way we consume medication. PBS News Hour, September 2014. https://www.pbs.org/newshour/health/tylenol-murders-1982
- Jefferies S, et al. Randomized controlled trial of the effect of regular paracetamol on influenza infection. Respirology (2016) 21, 470-477.
- Young P, et al. Acetaminophen for fever in critically ill patients with suspected infection. NEJM Dec 3 2015.
- Greenberg RS, Chen H, Hasday JD. Acetaminophen has limited antipyretic activity in criticall ill patients. J Crit Care. 2010 June; 25(2): 363e1-363e7.
- Tsaganos et al. Randomized, controlled, multicentre clinical trial of the antipyretic effect of intravenous paracetamol in patients admitted to hospital with infection. Â Br J Clin Pharacol. 2017 Apr;83(4)742-750.
- Suzuki S et al. Paracetamol therapy and outcome of critically ill patients: a multicenter retrospective observational study. Critical Care (2015) 19:162.
- Schortgen F. Fever control using external cooling in septic shock, a randomized controlled trial. Am J Respir Crit Care Med 2012 185:10:1088-1095.
- Young P, et al. “Acetaminophen for Fever in Critically Ill Patients with Suspected Infection”. NEJM. 2015. 373(23):2215-2224.
- Narayan K, Cooper S, Morphet J, Innes K. Effectiveness of paracetamol versus ibuprofen administration in febrile children: A systematic literature review. J Paediatr Child Health. 2017 Aug;53(8):800-807.
- Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, Peters TJ. Paracetamol and ibuprofen for the treatment of fever in children: the  PITCH randomised controlled trial. Health Technol Assess. 2009 May;13(27):iii-iv, ix-x, 1-163.
- Zampronio AR, Soares DM, Souza GEP “Central mediators involved in the febrile response: effects of antipyretic drugs†Temperature 2:4, 506-521; Oct/Nov/Dec 2015.
- Prajitha N, Athira SS, Mohanan PV. Pyrogens, a polypeptide produces fever by metabolic changes in the hypothalamus: Mechanisms and detections. Immunology Letters Vol 204, December 2018, 38-46.
- Zampronio AR, Soares DM, Souza GEP “Central mediators involved in the febrile response: effects of antipyretic drugs†Temperature 2:4, 506-521; Oct/Nov/Dec 2015.
- Vane JR, Flower RJ. Inhibition of prostaglandin synthetase in brain explains the anti-pyretic activity of paracetamol. Nature. 1972:240:410-411.

One comment on “Core IM: Mind the Gap on Acetaminophen/Fevers Pathophysiology and Patient Outcomes”
Brazilian listener here. Glad to know APAP would help in yellow scorpion sting via non PG-induced fever haha
Great show as always.
Cheers!
Comments are closed.