Podcast: Play in new window | Download
Subscribe: RSS
 By David Rhee MD, Greg Katz MD, Marty Fried MD, Shreya P. Trivedi MD || Illustration by Michael Natter MD || Audio Editing by Harit Shah. Quiz yourself on the 5 Pearls we will be covering:
By David Rhee MD, Greg Katz MD, Marty Fried MD, Shreya P. Trivedi MD || Illustration by Michael Natter MD || Audio Editing by Harit Shah. Quiz yourself on the 5 Pearls we will be covering:
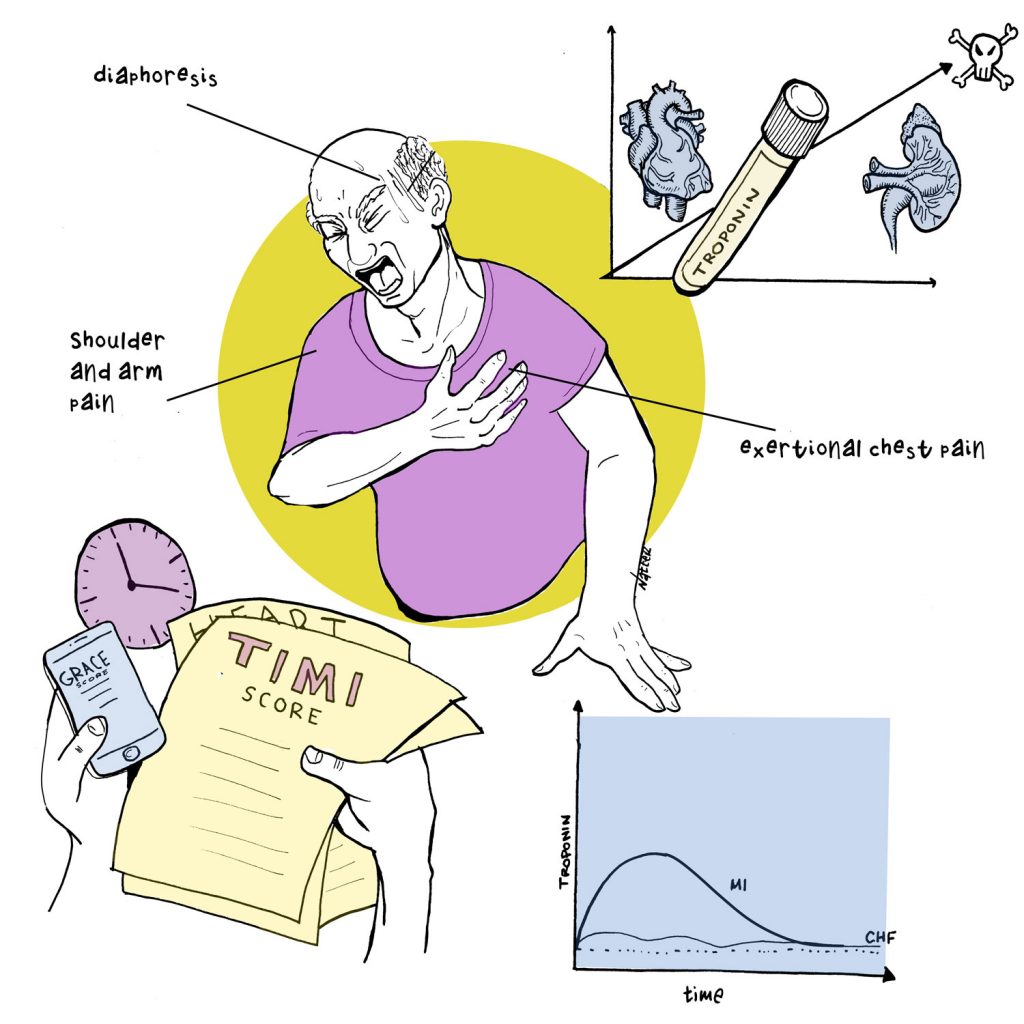
- What aspects of the history are concerning in a patient with a positive troponin? (4:00)
- What is the difference between the TIMI, GRACE, and HEART scores, and how should we use them in the evaluation of a patient with an elevated serum troponin? (8:42)
- Â How does the change in troponin over time help with diagnosis, and what should we consider in a patient with uptrending troponins but an unremarkable EKG? (14:48)
-  What can a “negative but detectable†troponin tell you about any patient, not just those with suspected ACS? (21:31)
- Pearls Recap (25:26)
- Throwback – what are the first-line medications for alcohol use disorder? (28:36)
Subscribe to CORE IM on any podcast app! Follow us on Facebook @Core IM || Twitter @COREIMpodcast || Instagram @core.im.podcast. Please give any feedback at COREIMpodcast@gmail.com.
Show Notes
Pearl 1: The Value of the Story
- While sensitive and specific to myocyte injury, the troponin is a piece of the clinical picture. Drill down into the HPI and risk factors to determine if this could be ACS.
- According to a paper in JAMA 2005, the history of chest pain radiating to the right arm/shoulder had the highest likelihood ratio for a myocardial infarction (LR 4.7), followed by radiation to bilateral arms and shoulders (LR 4.1). However, none of these elements alone or combination of elements in the history can reliably help us rule in or rule out ACS or AMI.
Pearl 2: Risk Stratifying Tools
- While there are various tools for risk-stratification, they should serve as adjuncts to your clinical impression and promote thoroughness as a structured checklist.
- The TIMI is the most historically validated for percent risk at 14 days of major adverse cardiac event.
- The GRACE score accounts for the physical exam and is most useful in those with heart failure or shock.
- The HEART score is most often used in the ED for undifferentiated chest pain as a tool to rule out ACS in low risk patients.
Pearl 3: Trending Troponins
- Low risk patients in ED (TIMI 0-1) can be ruled out for ACS with 2 negative troponins over 2 hours.
- Concerning troponins can be repeated as often as every 2-3 hours. Â
- When assessing the acuity of injury, think about troponin trends in terms of changes in log units (i.e. 0.05 to 0.07 vs 0.05 to 5).
- If suspicious for ACS but no ST changes on EKG, try posterior and right-sided EKG leads!
- The decision to trend troponins to peak is a case-by-case decision.
Pearl 4: Prognostication
- Regardless of the primary diagnosis, having elevated troponins in serum is abnormal and predicts worse outcomes in all patients.
- Having elevated troponins in patients with ESRD may not indicate ACS, but is still abnormal. It is likely due to the milieu of ESRD inflicting chronic microinjury to the myocardium.
Pearl 5: Throwback to Alcohol Use Disorder
- One study found that less than 9% of patients who needed treatment for AUD received a single prescription.
- First Line Agents: Naltrexone (1x/day dosing, cannot have cirrhosis or potential use of opioids in the future) and Acamprosate (3x/day dosing).
Transcript
M: Listen – trops can be easy to interpret for example when a long time smoker presents with sudden-onset crushing chest pain, EKG w/ ST elevations and the troponin is 20.  But the rubber meets the road when that exact same patient’s troponins are 0.04 and the chest pain is a bit vague and the EKG is nonspecific. So the real question is how do we interpret the troponins when the story isn’t so cut and dry?
S:  Can’t wait to dive deeper in this, but before we do that can we take a step back and ask what exactly is a troponin?
D: Yeah so this is super important to keep in mind when interpreting the test.  When we say troponin, we’re really referring to cardiac troponin I, which is a protein specific to cardiac myocytes and released when the cells are injured. So if you see a positive troponin, you know cardiac myocytes were injured.
S: But that injury can be from ischemia like in acute coronary syndrome or other injury. Think about things that cause injury  like toxic injury in sepsis or myocarditis, supply-demand mismatch like in heart failure, or ventricular wall stress with pulmonary emboli or valve dysfunction.
M: And just to make sure we’re all on the same page – what is a quote -unquote “positive troponinâ€Â
D: So that depends on the machine and the assay, but for the sake of this episode we are going to use our lab’s value of over 0.06. That threshold is the 99th percentile of a healthy population. Â
M: And just to get it out of the way, why aren’t we discussing CK-MB?
D: Well, before troponins, CK-MB was another marker for myocyte injury.  Many of us probably remember being taught in med school how the pharmacokinetics of CK-MB – the “quick up, quick down†line on the graph – may have theoretically been useful for re-infarction.  That never panned out and the consensus by cardiologists is that there’s no value added by CK-MB now that we have troponins. CKMB can also be falsely elevated in skeletal muscle injury. Troponins are just more sensitive and specific.
M: We’ll put up a link in our show notes to a 2017 paper in JAMA Internal medicine that does a great job reviewing the data behind CK-MB as well as a blueprint for a hospital QI project that can help providers move away from the test.  Alright, lets get on to our first pearl!
PEARL 1: The Story > Troponin
S: Let’s start with a case: 72F with history of hypertension and gout who presents to the ED with two episodes of acute CP while washing dishes, initial trop 0.05, which is below our lab’s cutoff
We spoke to several cardiologist and here’s what one would be thinking right now
Greg: So that trop is negative, but it’s also detectable and that’s a very important distinction to make when you’re thinking about a patient
M: That was Dr. Greg Katz, a 3rd year cardiology fellow at NYU. He has received numerous teaching awards so we really appreciated his input.  We’ll hear from him periodically during this podcast to get his take.
Greg: what I’m hearing is an elderly woman with gout and hypertension, so two coronary disease risk factors, who’s having chest pain with exertion because washing dishes for some people as the most strenuous exercise that they do and so already I’m thinking that this could be a plaque rupture
M: So that’s interesting. The trop was within normal limits for our lab and in the past I might have settled with calling it negative for MI.  But Greg points out that it’s still detectable, and he’s not ready to jump to any conclusions without a more nuanced approach.
S: Yeah, it actually seems like the least important aspect for his initial assessment seemed to be troponin. To him, this was a patient with enough risk factors and a plausible story of exertion that the trop didn’t comfortably “rule out†ACS for him.
Greg: that it’s, I, I’m going to keep falling back on. but it really is all about the story that you get and if you tell me that somebody has nausea and diaphoresis then and they’re having chest pressure at the same time. I’m thinking that it’s a little bit more likely to be an acute coronary syndrome, but I don’t know that they don’t have a viral gastroenteritis and they are having a little bit of pain from the vomiting that they’re about to do. It’s all about what the clinical stories and all of those things play play a role in how I am sort of internally adjusting and calibrating my pretest probability of a of a plaque rupture or an occluded coronary
D: So spend the extra few minutes to tease out the details of the story
Greg: Â Lots of people present weirdly with their coronary disease, diabetics, women, elderly patients, chronic kidney disease patients. How many patients with Mis have you taken care of that don’t have any of those factors like lots of people present strangely and law.
There are cultural sort of hurdles to understanding what someone’s symptoms are. There are like health literacy issues. There’s the fact that some people are just not conditioned to understand what’s going on with their body and they know they feel off and they can’t really.
M: I just love the point Greg is making here guys.  We hear all the time the phrase “patient is a poor historian†– and we forget that it’s not the patient’s job to tell us a narrative that fits neatly within a singular illness script.  That’s OUR job.
D: Yeah, and we absolutely need to consider the barriers that exist for a patient to tell their story.
S: Right, let’s say we have a patient without any of those barriers and we are able to get a clear chest pain history. What aspects of their chest pain story should raise our suspicion of ACS?
D: well we were always taught in med school how typical angina is substernal pressure that is triggered by exertion and relieved with rest or nitroglycerin. The other classic associations were radiation to the neck or left arm, diaphoresis, SOB, maybe some nausea or vomiting.
S: Right that’s what I was always taught, until one of my colleagues, brought up this old JAMA study that looked at thousands of cases of MI’s and their chest pain characteristics.  Take a guess as to what had the highest likelihood ratio to predict a true MI?
M: Exertional chest pain?
D: Diaphoresis?
S: Â ahh, fantastic guesses. Â Â Actually, exertional chest pain had a positive likelihood ratio of 2.4. Â Diaphoresis 2.0.
M:  Sheesh, so both findings do increase the chance of finding a MI, but I’ve been taught that likelihood ratios less than about 4 are really not that great !
S: So the finding with the strongest predictive power for myocardial infarction? Â Radiation to right arm or shoulder had a positive likelihood ratio of 4.7! And then radiation to both arms or shoulders came in at a likelihood ratio of 4.1
D/M: oh!
S: And symptoms with the lowest likelihood ratio? It’s not surprising. It’s the chest pain described as pleuritic, positional, reproducible, or sharp. Â
D: So our first pearl about troponins is actually: troponin isn’t everything. while it is specific to cardiac myocyte injury and the lab assays are really sensitive, it’s not the be all and end all of diagnosing ACS.  The cardiologists are really drilling into the background and the story to help put that troponin into a much larger context.
PEARL 2: Risk stratifying tools
S: So let’s go deeper into this case. We’re still in the ED.  It’s possibly, but not clearly, ACS. Definitely in a gray zone of sorts.  The first trop was negative but detectable in our lady with risk factors and exertional chest pain. You take a look at the EKG which shows nothing more than some T wave flattening – and obviously with no priors to compare to. Â
So what now?  What other tools that can help us objectively assess the risk of ACS in these “gray zone†cases?
M: Well we do have an alphabet soup of risk stratifying scores.  There’s the TIMI score, HEART score, and GRACE scores. But then I made the mistake of googling this and there’s like 7 other scores!  There’s the EDAC, there’s the Vancouver chest pain score – because obviously Canada needs to get involved with a scoring system here…
S: haha canada is always on top of things, I totally hear your frustration here Marty.  So I think what can help us is taking step back and discussing what exactly does it mean to ‘risk stratify’?
D: Yeah so risk stratifying is an important concept in chest pain.  The key questions are “Does this patient have blockages in her coronaries?  Is this presentation because of that? How quickly do we need to do a cath? And finally – how sick are they?†Every data point we collect will individually move our suspicion and concern for the patient up or down, and together the scores give us greater decision-making power to determine how we will proceed with treatment.
M: Alright, for the purposes of simplification we will focus our discussion on three of the most common scores – the TIMI, HEART, GRACE scores.
S: Great.  I think it’s worth pointing out that all of these tools can be used in patients who you suspect has ACS.  We need to appreciate that no single tool fits all scenarios. Each were validated using a particular registry – some included patients in the ED while others enrolled those who were already admitted.
M: So true.  Some of the information we’re about to discuss is visually represented in a recent issue of JACC that included a table of several different scores and their component parts.  We’ll link the paper in the show notes.
D:  So let’s start with the TIMI Score.  This is historically the most validated. It’s from a year 2000 publication, which is important to keep in mind because the troponin assay that was used back then was nowhere near as sensitive as the current tests – and they even counted patients with isolated CK-MB as having positive cardiac biomarkers!!
M: Unforgivable!
D: The GRACE Score similarly enrolled patients who were admitted w/ presumed ACS.  A major difference here is that the GRACE study tried to encompass the whole range of different ACS presentations and it takes hemodynamics and manifestations of heart failure into account. Because of this it’s more often used in patients who are critically ill.
And finally – the HEART Score. Â This was designed for the patient presenting to the ED with undifferentiated CP, may not even be ACS. Â In patient with LOW RISK of having ACS, the HEART score has been shown to outperform the other two tools.
M: So with that overview of the scores, let’s test drive these on our patient who may or may not have ACS?
D: Ok, let’s try the TIMI Score first.  So as I plug in her data, she’s 72, and since we didn’t get into meds yet let’s say she’s on daily ASA.  Her age, angina and ASA gives her a TIMI score of 3 which equals 13% risk of death or MI in the next 2 weeks.
M: Ok, what about the HEART Score?
D: For our patient, the HEART score is moderate, 5-6 points based on suspicious story, non ST elevation changes, age and 1 risk factor.  That moderate category equates to 12 to 16% risk of major adverse cardiac event in the next 6 weeks – so that’s similar.
M: And the GRACE?
D: Well GRACE is tough in this situation because it asks for specific vital signs and physical exam features like rales.  Remember this is often used for super sick patients so let’s skip it for now.
S: Sounds reasonable.  So both the HEART and TIMI scores are moderate – 13 to 15% of a major cardiac event isn’t something to ignore. It makes sense to admit her assess the trend in her troponin.  But, honestly, I probably would have done that without the tools.  It kind of feels like the risk stratifying tools did not add much more value.
M: we asked Greg how uses these tools like the TIMI or the HEART scores in his practice.
Greg: So I think that it’s. I, I use those risk scores as adjuncts to my clinical impression. I think that what the other thing they do is they force you to have a regimented approach to how you’re thinking about the patient and just by being forced to go through a checklist of various things. I think it really enforces a more complete history, taking in a more complete thought process and makes you miss fewer things
M: That’s a really valid point that Greg gives us.  We can be swept away sometimes in a patient’s story – sometimes getting side tracked by details that are initially difficult to tell if they are relevant or not.  The idea of these scores as a checklist is an interesting one.
S: I also think i learned the hard way that this allows us talk to our cardiology colleges in the same lingo. As an intern, I called cards on saturday morning and blurted out all these random bits of info about the patient and this cardiologist very nicely said back to me “Ok shreya, so what I think you are trying to tell me is that this is a middle aged female with x RF who presents with acute progressive CP with a TIMI score of 4 and therefore, you are asking me if we should cath her†and I was like YES, yes, that is exactly what I meant to ask.
D: haha its good to have some shared language
M: So let’s summarize our 2nd learning point: Tools like the TIMI HEART or GRACE scores can be helpful in risk stratify patients who may have ACS.  TIMI is the best studied and still most widely used, GRACE incorporates hemodynamics which the others don’t, and HEART is the new kid on the block and appears to be better at ruling out ACS than the others in the ED.  Despite these differences, in practice all three can be used for patients who present with a story that may be consistent with ACS and you are trying to determine how risky they are. But remember – these tools should only be used to supplement – not replace – our clinical reasoning. Â
S: Right because its true that patients with a low score can still have plaque rupture and patients with a high score might not.
PEARL 3: The troponin trend
S: Ok so our patient gets admitted for further evaluation. When should we get our second troponin? Do we have to wait 6-8 hours like we were taught in med school?  I’ve seen 4 hours, I’ve seen 12. What’s the right answer here?
Greg: So I, I think that if I have a troponin that is already on the concerning side, I make sure to repeat the next one pretty quickly and we know the kinetics of Troponin of the troponin in the blood after a coronary occlusion is that it will rise quickly and you get a lot of information by repeating a second troponin, an hour or two hours or three hours afterwards. And waiting for this eight hour period or 12 hour period or whatever is delaying your making a diagnosis and it’s, it’s just not necessary.
M: Yeah, a good example of this are the “rule out ACS†protocols in the ED, the ADAPT Trial being one of the more well-known examples.  They looked at patients and found that if they were low-risk, like TIMI Scores 0 or 1, they could be safely ruled out for ACS and discharged home if they had 2 negative troponins over just 2 hours.
S: So unfortunately our patient doesn’t qualify as “low-risk†based on TIMI. Let’s say there are no clinical changes and we get a troponin later at 6 hours, which comes back 0.07 which is now positive and slightly higher than her first troponin of 0.05. How do we interpret slight bump?
M: So this still could be anything. Â Key questions at this point are when did the chest pain start in relation to these labs, and how has the clinical situation changed. Â
D: Yeah exactly Marty.  This slow creep up might mean that we haven’t yet seen the inflection point in a plaque-rupture infarct that is happening before our eyes.  But it also can easily be seen in the low-grade supply-demand mismatch of a CHF exacerbation.
S: Well i hope there’s some other hx or E findings that help differentiate HF vs. ACS vs. myopericarditis but if it’s tricky, you can repeat the trop in 2-3 hrs and repeat EKG to eval for any dynamic ST changes
D:  Ok let’s try a different scenario. Let’s say our same patient from earlier has been experiencing stuttering chest pain on-off in the ED, and her second troponin a few hours later comes back and it’s now 5 instead. Â
M: Yeah so this is obviously quite different from the prior situation. Â A jump from 0.05 to 5 is a 100-fold increase! Most people are this point are calling for help. Â Cards is on the phone, cath lab staff are donning their lead. This is what these docs live for.
S: Oh yeah, the news team is assembling.  But let me throw a little curveball here. What if the repeat EKG  still doesnt ST changes?  I think we’re still doing everything we talked about with cath team, is there anything we are missing?
D: One of the pearls I learned from cardiologists is that a blocked left circumflex artery is the most common electrically silent MI, so if the clinical picture is suggestive of a real ACS event, like in this scenario the trop jumps from 0.05 to 5, but the standard EKG doesn’t show any ST changes, you should go searching for STE.   Get a posterior EKG and that can show a LCx STEMI. While you’re at it, you can also get a R-sided EKG for RCA occlusion. If you’ve never done them and don’t know where the leads go, you can just search for them on google images.
M: Or on our social media we have a 12LeadThursday series and we put together post  that walks you through this!
S: And this will definitely help our interventionalists, because if you can give them a culprit lesion they might plan the case around it.  For example, if they suspect a Left-circ or left coronary lesion they will quickly cannulate the RCA first and make sure there aren’t any surprises there before shooting the left main and spend more time opening up the left-sided blockage.
M: Awesome. Â Not gonna lie guys, I love saving our case patients. Â
D: Almost like we’re doing this in real life
M: Close.  Very close.  But, Ok, real question.  Let’s go back to the idea of trending troponinsthe first with a slow incremental rise in the clinically stable patient
S: let’s see what Greg had to say with the slowly uptrending troponin
Greg:if you have a heart failure exacerbation in a guy who just doesn’t take his lasix and he comes into the hospital and his trop is point, oh three. And then you check a couple of hours later and it’s like point oh six. And then you check a couple of hours later and it’s point one just it’s going up. But the trajectory of that increase is not a plaque rupture trajectory and your clinical history is not the clinical that’s suggestive of an acute coronary syndrome and so in a patient like that, I don’t really see what additional utility you’re getting from trending the super low level of Troponin until it’s officially going down.
S: So Greg’s point here really relates to the discussion in the first pearl.  If your pre-test probability for a plaque rupture is low based on their story, and the troponin is slowly creeping up, checking until the trop finally goes from point OH 91 (0.091) down to .090 isn’t really adding much, and given the etiology of this troponin leak hey it’s may very well go back to .092, which might be the most frustrating thing on this planet…
D: Hah that is the worst.  I totally hear what Greg is saying, and trust me I absolutely respect his opinion.  I do want to point out that some may feel like it’s good form to just trend to peak in all cases, having troponin in the blood is abnormal, and having an increase in troponin is still abnormal. There is no prospective study that has looked at this so it needs to be a case-specific decision.
M: For sure. Â Alright, what about the second lady who we valiantly saved in our hashtag-core-im-cathlab hashtag-whatup cardiotwitter
S: Ugh oh Marty is speaking in Twitter again, we need to hurry before things get ugly. Â
D:  So to answer Marty’s hashtag question, many advocate for trending troponins in patients post-cath.  Because if you take a graph of troponin over time and estimate the area under the curve, it can be used as a proxy for estimating infarct size and even mortality.  That information could be helpful for us in prognostication.
S: Nice prognostication is a great bridge to our next pearl.  But first, to summarize this section – the pattern of rise in troponin is useful in distinguishing who might needs immediate intervention.  And don’t forget about posterior EKG leads in electrically silent MIs – those are most commonly due to left circumflex infarctions!
PEARL 4: Trop as prognosticator
D: So let’s go allll the way back to our initial case.  Elderly woman who presents with chest pain and had a negative but detectable troponin.  Let’s take a completely different course and say that when you’re taking the history she also describes cough and a low-grade fever and you look at the XRay and she’s got a whopping left lower lobe pneumonia. Â
M: BOOM – we no longer care about the troponin, right?  I mean I’ve probably been guilty of leaving a detectable troponin off the final assessment of patients I’ve admitted with severe sepsis before – wait are we still using that term?  Either way, so what? We all know this isn’t due to a primary cardiac issue, so why do we care about a little type II MI?
D: So I hear you Marty, but a few important points here.  First, it’s important not to dismiss all sepsis cases as type II – critical illness could trigger plaque rupture or a stress cardiomyopathy which could show up as EKG changes and +troponins.
M: Fine, fair
S: And also Marty – the whole point of this Pearl is to drive home the idea that anyone with a detectable troponin, regardless of the etiology, has a higher risk of mortality than that same patient without a detectable troponin.
M: I sense a Greg comment coming…
Greg: Because even in healthy cohorts, people who have detectable troponins die younger and do worse and so the fact that you have at your Troponin that is detectable is in and of itself. Even if you are coming in with sepsis or you’re coming in with a stroke or you’re coming in with, you know, just leg pain. A positive troponin portends a worse outcome than a detectable proponent portends a worse outcome than an undetectable one. And there have been lots of studies looking at healthy cohorts of people with Troponin that are detectable in their blood and seeing how they do overtime and they die sooner than people who don’t.
S: Another group of patients where we hear this all the time for is patients with end stage renal disease.  I hear all the time from residents that the elevated troponin in a patient with ESRD is probably just quote – unquote for ‘false positive’
D:   My follow-up question is a false positive for what?!?  Troponin I is still specific to cardiac myocytes, a troponin still indicates myocardial damage. You don’t get false positives just because of ESRD – because troponin is renally cleared, it just takes longer to downtrend.
S: Right to hammer this home, any positive troponins in ESRD regardless of mechanism of injury have been shown to predict a 2 to 5-fold increase in all-cause mortality.
M: I guess you guys make a solid point.  So while these detectable troponin levels aren’t necessarily pointing us toward a primary cardiac etiology – and we really should convince ourselves that we’re not missing anything before we do that – they are clearly telling us something about these patients overall risk of death.
D: That’s right, after all cardiovascular disease accounts for roughly 50% of deaths in patients with chronic renal failure, so these patients are definitely sick even if they currently clinically stable.
M: I think a useful way to think about this group of patients is how you might sign them out to your night float colleague – Patient is “Xâ€-year old woman admitted for sepsis with detectable troponin on arrival thought to be type 2, now stable on antibiotics.  This communicates a higher level of risk, so when they get called for chest pain or hypotension or whatever they start with that leg up.
S: Â Great point, I like that example. Â
D: So in summary, don’t write off a detectable troponin in any setting!  These patient have a higher risk of mortality regardless of the etiology of troponin. Â
S: It is not an NBD situation!
Greg: I think about a Troponin as being either due to a coronary occlusion or not due to a coronary occlusion. And if you make that distinction and that’s the distinction that you’re trying to make in your mind, it makes you think about patients differently. And I think that all of the way that you teach people about diagnostic and clinical reasoning, it’s about giving. It’s about giving yourself away to frame a patient in your mind and get closer to making a diagnosis and closer to getting the right treatment for somebody, and so I’m alway s thinking about, do I think this one I see a Troponin I think do I think this patient has a coronary occlusion and if you frame it all in that way, it really simplifies your thinking quite a bit.
M: Thanks Greg.  And to review the takeaways we have the privilege of inviting our reviewer, Dr. Ernie Mazzaferri he is the Charles A. Bush Professor of Cardiovascular Medicine and medical director of the Ross Heart Hospital at the Ohio State University Wexner Medical Center.
Throwback Pearl: 1st line medications for alcohol use disorder (AUD)
D: For our throwback pearl let’s talk about our alcohol treatment podcast about treatment meds – What’s the first line treatment for AUD?
S: I really loved this podcast. I was struck by that statistic – I know its just in one paper but they found that less than 10% of patients who meet criteria for treatment for AUD get a single perscription. So my main change I’ve seen within myself is in the hospital. I am having that discussion more with patients admitted for alcohol withdrawal about their menu of options and feel more empowered to start naltrexone, as long as they dont have cirrhosis or a potential use of opioids in the future! I have had some really meaningful conversations with patients in the hospital.
M: I agree Shreya – my residents think I am a broken record with this, but I discuss medications to treat alcohol use disorder with everyone who i think might benefit from them.  We should also mention that acamprosate is the other consensus first-line medication, but the tricky thing is that it’s dosed three times daily. Â
S: Â Yeah I didn’t think of acamprosate as a first line med, but the NNT of 12 Â to prevent any drinking helped me think about it differently. I haven’t started it yet but maybe paitents who have potential use of opioids in the future and with shared decision making that they are okay with three times a day dosing, I might start it.
References
- Zimmerman, D. L. (1982). Requiem for a Heavyweight: A Farewell to Warren and Brandeis’s Privacy Tort. Cornell L. Rev., 68, 291. https://www.ncbi.nlm.nih.gov/pubmed/19015414
- Braunwald, E., Antman, E. M., Beasley, J. W., Califf, R. M., Cheitlin, M. D., Hochman, J. S., … & Pepine, C. J. (2000). ACC/AHA guidelines for the management of patients with unstable angina and non–ST-segment elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina). Journal of the American College of Cardiology, 36(3), 970-1062. http://www.onlinejacc.org/content/36/3/970/T9
- Christenson, R. H., Duh, S. H., Sanhai, W. R., Wu, A. H., Holtman, V., Painter, P., … & Morris, D. L. (2001). Characteristics of an albumin cobalt binding test for assessment of acute coronary syndrome patients: a multicenter study. Clinical Chemistry, 47(3), 464-470. https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2017/08/14/12/31/eliminating-creatine-kinase-myocardial-band-testing
- Swap, C. J., & Nagurney, J. T. (2005). Value and limitations of chest pain history in the evaluation of patients with suspected acute coronary syndromes. Jama, 294(20), 2623-2629. https://www.ncbi.nlm.nih.gov/pubmed/16304077
- Wilson, P. W., & D’Agostino, R. B. (2016). No One Size Fits All: Scoring Risk of In-Hospital Death After Myocardial Infarction. https://www.ncbi.nlm.nih.gov/pubmed/?term=27491908
- Sakamoto, J. T., Liu, N., Koh, Z. X., Fung, N. X. J., Heldeweg, M. L. A., Ng, J. C. J., & Ong, M. E. H. (2016). Comparing HEART, TIMI, and GRACE scores for prediction of 30-day major adverse cardiac events in high acuity chest pain patients in the emergency department. International journal of cardiology, 221, 759-764. https://www.ncbi.nlm.nih.gov/pubmed/27428317
- Reaney, P. D., Elliott, H., & Cooper, J. (2016). A Comparison Of The Heart, Timi And Grace Scores In The Prediction Of A Major Adverse Cardiac Event (mace) In Patients Presenting With Undifferentiated Cardiac Chest Pain: A Prospective Cohort Study In A Uk Population. Emerg Med J, 33(12), 916-917. https://emj.bmj.com/content/33/12/916.2
- Poldervaart, J. M., Langedijk, M., Backus, B. E., Dekker, I. M. C., Six, A. J., Doevendans, P. A., … & Reitsma, J. B. (2017). Comparison of the GRACE, HEART and TIMI score to predict major adverse cardiac events in chest pain patients at the emergency department. International journal of cardiology, 227, 656-661. https://www.internationaljournalofcardiology.com/article/S0167-5273(16)33282-X/fulltext
- Antman, E. M., Cohen, M., Bernink, P. J., McCabe, C. H., Horacek, T., Papuchis, G., … & Braunwald, E. (2000). The TIMI risk score for unstable angina/non–ST elevation MI: a method for prognostication and therapeutic decision making. Jama, 284(7), 835-842. https://www.ncbi.nlm.nih.gov/pubmed/10938172
- Than, M., Cullen, L., Aldous, S., Parsonage, W. A., Reid, C. M., Greenslade, J., … & Troughton, R. (2012). 2-Hour accelerated diagnostic protocol to assess patients with chest pain symptoms using contemporary troponins as the only biomarker: the ADAPT trial. Journal of the American College of Cardiology, 59(23), 2091-2098. https://www.ncbi.nlm.nih.gov/pubmed/22578923
- Apple, F. S., Murakami, M. M., Pearce, L. A., & Herzog, C. A. (2002). Predictive value of cardiac troponin I and T for subsequent death in end-stage renal disease. Circulation, 106(23), 2941-2945. https://www.ncbi.nlm.nih.gov/pubmed/12460876

One comment on “Core IM: 5 Pearls on Troponin”
Great episode. There has actually been a more recent 2015 JAMA meta-analysis on LRs for chest pain characteristics in 2015. Turns out no “typical†symptom is better than LR 2.6 (radiation to both arms)- much less 4.7 from the older paper.
search “chest pain LR ACS†-> https://www.grepmed.com/images/3046
Comments are closed.