Commentary by Dr. Daniel Labovitz, Director of the NYU Stroke Center
After an 8-year hiatus, the American Heart Association/American Stroke Association has at last published a fresh set of guidelines on the management of acute spontaneous intracerebral hemorrhage (ICH) [Stroke 2007: DOI: 10.1161/STROKEAHA.107.183689]. ICH represents between 10 and 20% of all first strokes, depending on the population, but carries a mortality rate of 35% to 50%, with hemorrhage volume, hemorrhage location, intraventricular extension and age all contributing independently to the risk of death. Unfortunately, our therapeutic options have not changed substantially since the last set of guidelines came out in 1999. However, the new guidelines do provide a succinct overview of the literature and reflect evolving expert opinion based on pilot studies and observational studies. The paragraphs below describe some highlights.
Since the last set of guidelines was published there have been only two phase 3 clinical trials for acute hemorrhage management and both were negative. The STICH trial [Lancet 2005;365:387-397] showed no benefit for early surgical hemorrhage evacuation (within 24 hours of enrollment) as compared to routine care (including later surgical evacuation); however secondary analysis suggested there might be a benefit to early evacuation if the hematoma is <1 cm from the surface. The results of the phase 3 FAST trial of factor VII for acute ICH were not available for discussion in the guidelines but the phase 2 trial is discussed. We now know that the phase 3 trial was negative (unpublished except for a February 2007 press release), showing no benefit for disability or mortality at 3 months, although hemorrhage size was significantly reduced.
Although no important trials on blood pressure management in acute ICH have been published since the last set of guidelines came out, the discussion of blood pressure management is substantially expanded and the recommendations are slightly more nuanced. A series of studies have shown that some hematomas continue to expand in the first hours after onset, although expansion doesn’t continue beyond 24 hours in the absence of a coagulopathy. Theoretically, aggressive blood pressure reduction might reduce the risk of hematoma expansion; on the other hand, blood pressure reduction might lead to infarction of tissue with reduced circulation due severe local mass effect (although no such “penumbra” of tissue has been demonstrated on PET). The original guidelines recommended keeping the MAP <130 in acute ICH patients based on such reasoning. The new guidelines are effectively no different, recommending MAP <130 or SBP <180 and, for the first time, suggesting that pressure should be maintained high enough to maintain a cerebral perfusion pressure >60. The guidelines do not address how long the parameters should apply.
Prophylaxis against venous thrombo-embolism is addressed. The old guidelines simply stated that pneumatic compression devices reduce the risk of pulmonary embolism but made no formal recommendation. Now pneumatic compression devices are a class 1 recommendation; furthermore, subcutaneous heparin “may be considered…3-4 days from onset.”
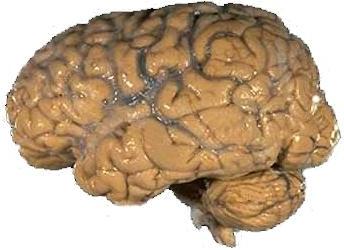
Image of human brain from NIH, courtesy of Wikimedia Commons.
