Faculty Peer ReviewedÂ
While everyone is talking about the passage of further work hour restrictions, now limiting interns to 16-hour shifts in hopes of preventing or at least reducing “medical errors” [1] let’s take a look at the other news about prevention and screening that has come out this week.
Last week in Primecuts, we read about the controversies surrounding screening for prostate cancer. This week, the Annals re-explored the idea of screening for testicular cancer [2].   The authors were searching for new evidence to update the 2004 United States Preventive Services Task Force guidelines, which recommend against it (grade D). None of the ultimately reviewed articles met all the initial inclusion criteria, mostly because many studies exploring testicular cancer are based on symptomatic patients, who by definition cannot belong to a screening population. Nonetheless, there were two notable articles that found potential correlations between both testicular microlithiasis and XIST gene methylation with testicular cancer. The authors also reviewed the literature for any evidence of harm from testicular cancer screening and found none. In the end, they felt that there was no evidence to change current guidelines. You can actually comment on the screening guidelines here; I’m agreeing with the USPSTF on this one.
The same journal also looked at the cost-effectiveness of stool DNA testing to screen for colorectal cancer, and found that, evaluating the $350 test at 3-year intervals in two microsimulation models, there was no benefit to this approach [3]. Based on the analysis, if the test decreased to sixty dollars or if adherence rates improved by at least 50% as compared to current testing strategies it would be cost-effective. While in theory one could argue this is plausible given the noninvasive nature of the test, in reality it was already compared to fecal occult blood testing (FOBT) which is also noninvasive and did not measure up. Also recall that this test, though 83% sensitive, screens for a finite number of gene abnormalities, which would seem to be more helpful in diagnosis than screening. While I am in full support of a less invasive test, it does not seem to me that there is enough data to support this newer method, though it is on the American Cancer Society’s list of screening alternatives.
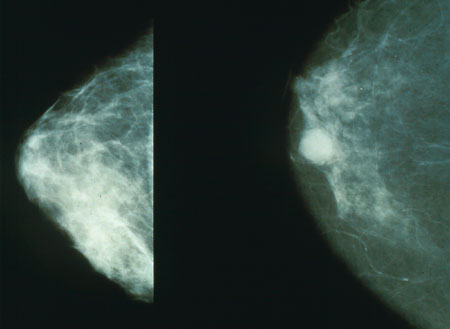
Lastly, we revisit the debate on mammograms. While the American Cancer Society recommends screening mammograms for all women over 40, the USPSTF does not cite enough evidence to justify screening mammograms for women ages 40-49 (grade C). An online publication from Cancer this week reviewed a cohort of more than 600,000 women in Sweden to examine the effectiveness of screening mammograms in younger women [4]. This study found that as compared to unscreened women screening women ages 40-49 resulted in a statistically significant 26% reduction in breast cancer death rate. While the overall number needed to screen was 1252, sub-group analysis showed a greater percentage of these cases came from women aged 45-49, which makes sense given breast cancer’s increasing prevalence with age. The study attempted to account for lead time bias, but some critics still feel that this may not have been sufficiently addressed [5].
This comes fresh on the heels of a study published in NEJM last week that questioned the extent of benefit derived from mammograms. The study looked at forty thousand women in Norway; by virtue of their currently expanding public health system researchers were able to directly compare mammography-screened and unscreened populations [6]. They found that, for women aged 50 to 69, there was a 10% relative reduction in mortality attributable to screening, versus previous numbers which estimate this value to be as high as 25% [7]. The authors agree that breast cancer mortality is much improved now as compared to earlier but cite multidisciplinary teams and improvement in treatment strategies as the main reason for this, more so than the benefit of screening.
Enough about cancer. Let’s talk about another top-ten cause of mortality: heart disease. In a July Primecuts, our own Dr. Hormozdi commented on the use of statins for primary prevention, citing the JUPITER study. He concluded that more information is needed before changing clinical practice. Well, maybe some of that information has arrived. Circulation just published a study looking at the cost-effectiveness of statin therapy, specifically including hs-CRP screening [8]. The simulation model found that the current set of ATP guidelines is likely optimal. However, when small changes in contributing factors were tested, such as a decreased side effect profile for statins, or a higher adherence rate to statin therapy in the face of an elevated hs-CRP level, the model showed that an alternative approach may actually be the best course. Options for this approach then include treating a patient with a Framingham risk score of 10-15% with statins, or only prescribing statins to patients who have documented elevated hs-CRP levels, to name some examples. Again, I don’t think there’s anything here that should change management today, but it does continue to raise some interesting questions about our understanding of risk factors for cardiovascular disease.  To help guide us, there is an online model from the Stanford website that weighs in these different variables based on you iniput and subsequetnly provides you wiht the best screening strategy for you patient. What’s especially interesting to me is how this study was portrayed to the public as showing a fairly clear economic benefit to statins, at least according to Time magazine [9], reiterating the importance of good communication directly between physicians and patients.
 This week’s Primecuts ends with a reminder to get your flu shot! Speaking of the flu, BMJ published a Chinese study looking at oseltamivir treatment early in the H1N1 pandemic [10]. It found that, in the 1300 patients treated, oseltamivir protected against radiographic development of pneumonia, and when given within 2 days of symptom onset, decreased length of fever and load of viral RNA shedding. Interestingly, the study indicated that H1N1 may have a longer shedding time than traditional flu, and that there was some benefit derived from oseltamivir therapy even after 48 hours had passed. You, of course, can help with prevention by getting your flu shot this week.
 Dr. Tummala is a 2nd year resident at NYU Langone Medical Center
Peer Reviewed by Michael Tanner, MD, Associate Editor, Clinical Correlations
Image courtesy of Wikimedia Commons.
 References:
1. Shorter work hours approved for medical residents. The New York Times. 2010 Sept 29; Money and Policy. Web. http://www.nytimes.com/aponline/2010/09/29/health/policy/AP-US-MED-Doctors-Work-Hours.html?ref=health.
2. Lin K, Sharangpani R. Screening for testicular cancer: an evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2010 Sept;153(6):396-399. Print. http://www.annals.org/content/153/6/396.abstract.
3. Lansdorp-Vogelaar I, Kuntz KM, Knudsen AB, Wilschut JA, Zauber AG, Ballegooijen. Stool DNA testing to screen for colorectal cancer in the Medicare population: A cost-effectiveness analysis. Ann Intern Med. 2010 Sept;;153(6):368-377. Print. http://www.annals.org/content/153/6/368.abstract.
4. Hellquist BN, Duffy SW, Abdsaleh S, et al. Effectiveness of population-based service screening with mammography for women ages 40 to 49 years: Evaluation of the Swedish Mammography Screening in Young Women (SCRY) cohort. Cancer. Published online Sept 29, 2010. Web. http://onlinelibrary.wiley.com/doi/10.1002/cncr.25650/abstract.
5. Kolata, G. Mammogram benefit seen for women in their 40s. The New York Times. 2010 Sept 29; Research. Web. http://www.nytimes.com/2010/09/30/health/research/30mammogram.html?emc=eta1
6. Kalager M, Selen M, Lanfmark F, Adami HO. Effect of screening mammography on breast-cancer mortality in Norway. N Engl J Med. 2010 Sept;363:1203-10. Print. http://www.nejm.org/doi/full/10.1056/NEJMoa1000727.
7. Stein, R. New study questions mammograms. The Washington Post. 2010 Sept 23; Health. Web. http://voices.washingtonpost.com/checkup/2010/09/new_study_questions_mammograms.html.
8. Lee KK, Cipriano LE, Owens DK, Go AS, Hlatky MA. Cost-effectiveness of using high-sensitivity C-reactive protein to identify intermediate- and low-cardiovascular-risk individuals for statin therapy. Circulation. 2010 Sept;122(13):1478-1487. Web. http://circ.ahajournals.org/cgi/content/abstract/CIRCULATIONAHA.110.947960v1.
9. Park, A. Study: Putting more people on cholesterol-lowering drugs could save money. Time Healthland. 2010 Sept 27. Web. http://healthland.time.com/2010/09/27/statins-for-all-it-could-save-money/
10. Yu H, Liao Q, Yuan Y, et al. Effectiveness of oseltamivir on disease progression and viral RNA shedding in patients with mild pandemic 2009 influenza A H1N1: opportunistic retrospective study of medical charts in China. BMJ. 2010 Sept;341:c4779. Print. http://www.bmj.com/content/341/bmj.c4779.abstract.

 By Lakshmi Tummala, MD
By Lakshmi Tummala, MD
One comment on “Primecuts – This Week In The Journals”
Please look at recent JAMA article: http://jama.ama-assn.org/cgi/content/full/294/9/1025 for neurolocognitive effects of night call versus alcohol. It is very interesting. Loren
Comments are closed.