Peer ReviewedÂ
Beginning in medical school, in between lectures on biochemistry, anatomy, and physiology, students begin to learn the physical exam and its role in the diagnosis of medical conditions. Some of these findings are grouped into eponymous triads, named after the physicians of yore who first identified these findings and the diagnoses they suggest. How useful, though, are these triads in modern medical practice today? In this article, I will explore the recent evidence evaluating a dyad of triads and provide some history on the physicians whose names live on through these groupings.
Beck’s Triad
In 1935, thoracic surgeon Dr. Claude Schaeffer Beck published an article in the Journal of the American Medical Association describing how to diagnose cardiac tamponade in the setting of a pericardial effusion. In Dr. Beck’s paper, two triads were described, one for “acute compression†and the second for “chronic compression.†Beck’s triad of acute compression is the one we commonly learn today, describing pericardial tamponade as presenting with “(1) a falling arterial pressure, (2) a rising venous pressure and (3) a small quiet heart†[1]. Or, as we would describe: hypotension, elevated jugular venous pressure, and muffled heart sounds [2]. Beck’s triad of chronic compression consisted of ascites, elevated jugular venous pressure, and muffled heart sounds [1]. I would recommend going here to watch a video of jugular venous pulsation in cardiac tamponade.
For the purposes of this article, I will focus on Beck’s triad of acute compression as a way to diagnose acute cardiac tamponade. A 2007 systematic review published in JAMA evaluated eight studies to determine the group’s sensitivity for the diagnosis of tamponade. The sensitivities of the individual components were as follows: hypotension 26 ± 10%, diminished heart sounds 28 ± 7%, and elevated jugular venous pressure 76 ± 14% [3]. There was no estimation of the sensitivity for the entire triad of symptoms, but it is likely poor given the low individual sensitivities of hypotension and muffled heart sounds.
A more recent 2017 retrospective chart review of patients presenting to two emergency departments examined the sensitivity of Beck’s triad in 153 patients. While not a systematic review, the study did assess for the presence of Beck’s triad in each patient. The authors found that Beck’s triad was 0% (95% CI 0-19%) sensitive for the diagnosis of pericardial effusion, and that the sensitivity of any one of the triad’s components for identifying tamponade was 50 ± 22% [2].
Given the poor sensitivities of these findings, what is the most useful way to rule in or rule out tamponade at the bedside? In the 2007 systematic review, the most important physical exam finding to diagnose cardiac tamponade was a pulsus paradoxus greater than 10 mmHg with a sensitivity of 82 ± 10%. This finding had a positive likelihood ratio of 3.3 (95% CI 1.8-6.3), and a negative likelihood ratio of 0.03 (0.01-0.24). A higher cutoff for pulsus paradoxus provides even greater ability to detect tamponade. A pulsus paradoxus greater than 12 had a positive likelihood ratio of 5.9 (95% CI 2.4-14) [3]. Pulsus paradoxus less than 10 argues strongly against the diagnosis of pericardial tamponade.
Claude Schaeffer Beck was born in 1894 and trained in neurosurgery at Harvard and Johns Hopkins Hospital before obtaining training in cardiovascular surgery at the University Hospitals of Cleveland. Besides his eponymous triad, he is also famous for performing the first successful defibrillation in 1947 and becoming the first professor of cardiovascular surgery in the United States in 1952. He passed away in 1971 [4].
Charcot’s Cholangitis Triad
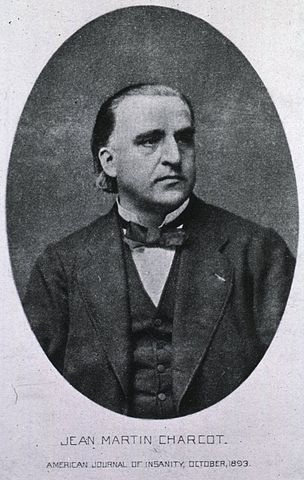
In 1877, Jean-Martin Charcot, a French physician practicing at the Salpêtrière in Paris, presented to a group of physicians his criteria to diagnose acute cholangitis, in a talk titled “Leçons sur maladies du foie, des voies biliaires et des reins, faires a la faculte de medecine†[5,6]. Or, in English, as per Google Translate: “Lectures on Diseases of the Liver, Bile Ducts, and Kidneys, made at the Faculty of Medicine.†These criteria were fever, jaundice, and right upper quadrant pain [5,6]. Charcot’s criteria came to be known as Charcot’s cholangitis triad, to separate them from his neurological triad for multiple sclerosis: nystagmus, intention tremor, and scanning speech [7].
How useful is Charcot’s cholangitis triad in modern practice? Multiple studies have been done looking at the sensitivity and specificity. This is of vital importance, given the need for urgent treatment of this disease [8]. A 2017 systematic review found 16 suitable studies in the literature. Sensitivity was calculated from all 16 studies, while specificity could only be calculated from three of them. The triad had a poor sensitivity of only 36.3%, with a stronger specificity of 93.2% [8]. This leads to a positive likelihood ratio of 5.3, and a negative likelihood ratio of 0.68. Of note, there was great heterogeneity in the individually reported sensitivities, ranging from 7.7% in a cohort of patients with mild disease, to 72% in a sicker cohort [8]. Overall, Charcot’s cholangitis triad appears more useful for ruling in a diagnosis of acute cholangitis, but is likely to miss many other cases.
In 1959, Drs. Benedict M. Reynolds and Everett L. Dargan of the Bronx Municipal Hospital Center reported a case series of patients with acute cholangitis who benefited from emergent surgical biliary decompression. They diagnosed these patients with what they termed acute obstructive cholangitis. These patients all had “the well known triad of chills and fever, jaundice, and right upper quadrant abdominal pain or tenderness,†but noted that “the addition of lethargy or mental confusion and shock to this triad†represented acute obstructive cholangitis as opposed to acute cholangitis [9]. Today, we refer to this as Reynolds’ pentad, which we associate with suppurative cholangitis. However, in the systematic review above, the sensitivity of Reynolds’ pentad across nine of the studies was 4.82% [8].
Dr. Charcot was born in 1825 and received his medical doctorate from the University of Paris in 1853, before working at the Salpêtrière [7,10]. While many in medicine are familiar with Dr. Charcot for his cholangitis triad, he is better known for his contributions to neurology, and is often called “the father of neurology†[7]. Charcot was a pathologist and gifted teacher who influenced many now-famous physicians, including Sigmund Freud and Charles Babinski [7,10]. Among the many diseases he helped characterize are multiple sclerosis, Charcot-Marie-Tooth Disease, amyotrophic lateral sclerosis, and Charcot’s joint. Dr. Charcot passed away in 1893 [7].
Dr. Reynolds graduated from New York University School of Medicine in 1948 and went on to practice surgery. Among other titles throughout his career, he was chairman of Surgery at Fordham Hospital from 1976 to 1982 [11]. At the time his paper was published, Dr. Reynolds practiced at The Bronx Municipal Hospital Center, which consisted of Jacobi Hospital and Van Etten Hospital, a 500-bed sanitarium for the chronic care of patients with tuberculosis [12]. Dr. Reynolds died in 2019 at the age of 94 [11].
Dr. Joshua Novack is a first-year resident in the NYU Langone Internal Medicine Residency
Peer Reviewed by David Kudlowitz, MD, assistant professor, Department of Medicine (Division of General Internal Medicine) and associate editor for Clinical Correlations
Image courtesy Wikimedia Commons
References
- Beck CS. TWO CARDIAC COMPRESSION TRIADS. JAMA J Am Med Assoc. 1935;104(9):714. doi:10.1001/jama.1935.02760090018005
- Stolz L, Valenzuela J, Situ-LaCasse E, et al. Clinical and historical features of emergency department patients with pericardial effusions. World J Emerg Med. 2017;8(1):29-33. doi:10.5847/wjem.j.1920-8642.2017.01.005. Accessed 10/26/2020. http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.1935.02760090018005
- Roy CL, Minor MA, Brookhart MA, Choudhry NK. Does This Patient With a Pericardial Effusion Have Cardiac Tamponade? JAMA. 2007;297(16):1810. doi:10.1001/jama.297.16.1810. Accessed 10/26/2020. http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.297.16.1810
- Dittrick Medical History Center. Claude Beck, defibrillation and CPR. Case Western Reserve University College of Arts and Sciences Dittrick Medical History Center. Accessed October 26, 2020. https://artsci.case.edu/dittrick/online-exhibits/explore-the-artifacts/claude-beck-defibrillation-and-cpr/
- Jean-Martin Charcot. Lecons sur les maladies du foie, des voies biliaires et des reins, faites a la faculte de medecine – – Jean-Martin Charcot – Hachette Bnf – Grand format – Le Hall du Livre NANCY.; 1877. Accessed October 29, 2020. https://halldulivre.com/livre/9782012979116-lecons-sur-les-maladies-du-foie-des-voies-biliaires-et-des-reins-faites-a-la-faculte-de-medecine-jean-martin-charcot/?autreEdit=true
- Lipsett PA, Pitt HA. Acute cholangitis. Front Biosci J Virtual Libr. 2003;8:s1229-1239. doi:10.2741/881. Accessed October 29, 2020. https://www.bioscience.org/2003/v8/s/881/fulltext.htm
- Kumar DR, Aslinia F, Yale SH, Mazza JJ. Jean-Martin Charcot: The Father of Neurology. Clin Med Res. 2011;9(1):46-49. doi:10.3121/cmr.2009.883. Accessed October 29, 2020. http://www.clinmedres.org/content/9/1/46
- Rumsey S, Winders J, MacCormick AD. Diagnostic accuracy of Charcot’s triad: a systematic review. ANZ J Surg. 2017;87(4):232-238. doi:10.1111/ans.13907. Accessed October 29, 2020. https://onlinelibrary.wiley.com/doi/abs/10.1111/ans.13907
- Reynolds BM, Dargan EL. Acute obstructive cholangitis; a distinct clinical syndrome. Ann Surg. 1959;150(2):299-303. doi:10.1097/00000658-195908000-00013. Accessed October 29, 2020. https://doi.org/10.1016/S0039-6109(16)45285-0
- Jean-Martin Charcot | French neurologist. Jean-Martin Charcot. Published August 12, 2020. Accessed October 29, 2020. https://www.britannica.com/biography/Jean-Martin-Charcot
- Benedict Reynolds Obituary (1925 – 2019) – The Journal News. The Journal News. Published April 16, 2019. Accessed October 29, 2020. https://obits.lohud.com/amp/obituaries/lohud/192398762
- NYC Health + Hospitals. Jacobi Hospital History. Jacobi Hospital History. Accessed October 29, 2020. https://www.nychealthandhospitals.org/jacobi/history/