Faculty Peer Reviewed
Obesity is defined as a body mass index (BMI) of ?30 kg/m2. The rate of obesity in the United States has skyrocketed over the last several decades, becoming a disease of epidemic proportions. According to the Centers for Disease Control and Prevention, in 2009, 32 states had a prevalence of obesity of ?25%, while 9 of these states had a prevalence of ?30%. It has been estimated that the economic costs of treating obesity and its complications, including type 2 diabetes mellitus, heart disease, stroke, osteoarthritis, certain cancers, obstructive sleep apnea, and depression costs the United States approximately $100 billion annually.[1] Over the past several years, bariatric surgery has soared in popularity as an effective weight loss modality. In fact, the NYU Langone Medical Center and Bellevue Hospital Center have been designated Bariatric Surgery Center of Excellence. Although several studies have shown a mortality benefit with bariatric surgery, a 2011 study published in JAMA refutes this claim, posing the question: is there really a long-term mortality benefit with bariatric surgery?
Several studies have demonstrated a relationship between weight loss from bariatric surgery and improved survival when compared to medical management for obesity. The Swedish Obese Subjects study (SOS) was a prospective, matched, surgical interventional trial with 4047 patients (71% female) with an average age of 47 years, and an average follow-up of 10.9 years.[2] After 10 years, the control cohort had an average weight loss of ± 2%, while the surgery cohort had an average weight loss of 14-25%, depending on surgery type, with a decrease in mortality of 21% (absolute risk reduction 1.3%). Importantly, this study was not powered to elucidate the mechanism through which mortality was decreased by bariatric surgery.
A second study, this one a retrospective analysis, had 7925 patients (85% female), with an average age of 39 years, and a mean follow up of 7.9 years.[3] This study demonstrated a 40% decrease in mortality (absolute risk reduction 1.5%) in the surgery cohort, and importantly, this study stratified the mortality benefit. There was a 56% decrease in mortality from coronary artery disease, a 92% decrease in mortality from diabetes, and a 60% decrease in mortality from cancer. Interestingly, death not caused by disease was 58% higher in the surgery cohort. Both of these studies demonstrated a significant decrease in long-term mortality for obese patients who underwent bariatric surgery compared to matched obese patients who were treated with medical management.
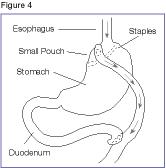
The long-term decrease in mortality must be compared with the perioperative mortality rate from bariatric surgery. According to the LABS Consortium, the 30-day mortality rate for bariatric surgery is 0.3% (0% for laparoscopic adjustable gastric banding, 0.2% for laparoscopic Roux-en-Y gastric bypass, and 2.1% for open Roux-en-Y gastric bypass).[4] Considering these findings, the long-term mortality benefit for laparoscopic adjustable gastric banding and laparoscopic Roux-en-Y gastric bypass exceeds the perioperative mortality for both operations, while the perioperative mortality for open Roux-en-Y gastric bypass surpasses the long-term mortality benefit from the weight loss accomplished by the surgery. Open bariatric surgery, however, constitutes less than 10% of all bariatric surgery performed in the United States.[5] Perioperative mortality rate must be carefully considered when recommending bariatric surgery to a patient.
While the aforementioned studies have demonstrated a 21-40% reduction in long-term mortality after bariatric surgery compared to matched controls prescribed medical management for obesity, a 2011 study in JAMA by Maciejewski and colleagues did not demonstrate a statistically-significant mortality benefit for bariatric surgery. The study was a retrospective analysis of 1695 patients (74% male) in Veterans Affairs medical centers, with an average age of 50 years, and an average follow-up of 6.7 years.[6] With propensity-matched controls and after Cox regression, bariatric surgery was not found to have a decreased long-term mortality rate when compared to medical management for obesity (hazard ratio of 0.83, 95% confidence interval of 0.61-1.14). The study’s authors claim that their surgery cohort was at high risk because the majority of patients were men, at an older average age, and with higher average BMI than previous studies with a similar endpoint. In the 2 previously examined studies, the majority of patients were female, with a younger average age, and lower average BMI. Also, the BMI of the patients in the VA surgery group was 47.4 kg/m2 compared to 42.0 kg/m2 in the nonsurgical controls. The lack of mortality benefit found with bariatric surgery in such a high-risk cohort may be due to the advanced comorbid illnesses that the patients already had due to obesity, indicating that for older and sicker patients, bariatric surgery does not confer a mortality benefit; the benefit is found in younger and healthier patients who have yet to experience end-organ dysfunction from obesity and its related complications.
Historically, bariatric surgery has been associated with improvements in quality of life, morbidity, and, most importantly, mortality. It is essential to compare the perioperative mortality rate with the long-term improvement in mortality conferred by bariatric surgery to ultimately determine the mortality benefit of surgery. Recent data, however, have shown no mortality benefit for bariatric surgery in high-risk obese patients. The lack of mortality benefit can likely be explained by irreversible end-organ damage, which could have been prevented had surgery been done at a younger age. This suggests that a more careful examination of comorbid illnesses and end-organ dysfunction should be performed before recommending patients for bariatric surgery in order to more carefully select those patients who will have a mortality benefit from surgery. More studies on the long-term risks and benefits of bariatric surgery are sure to be published, improving the quality of evidence assessing the long-term implications of bariatric surgery.[7]
Marc O’Donnell is a 4th year student at NYU School of Medicine
Peer reviewed by Manish Parikh, MD, Assistant Professor, Department of Surgery, NYU Bariatric Surgery Associates
Image courtesy of Wikimedia Commons
References
1. Ludwig DS, Pollack HA. Obesity and the economy: from crisis to opportunity. JAMA. 2009;301(5):533-535. http://jama.ama-assn.org/content/301/5/533.full
2. Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741-752. http://www.nejm.org/doi/full/10.1056/NEJMoa066254#t=articleTop
3. Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753-761. http://www.nejm.org/doi/full/10.1056/NEJMoa066603#t=articleTop
4. Longitudinal Assessment of Bariatric Surgery (LABS) Consortium. Flum DR, Belle SH, King WC, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361(5):445-454. http://www.nejm.org/doi/full/10.1056/NEJMoa0901836#t=articleTop
5. DeMaria EJ, Pate V, Warthen M, Winegar DA. Baseline data from American Society for Metabolic and Bariatric Surgery-designated Bariatric Surgery Centers of Excellence using the Bariatric Outcomes Longitudinal Database. Surg Obes Relat Dis. 2010;6(4):347-355. http://www.sciencedirect.com/science/article/pii/S1550728909007709
6. Maciejewski ML, Livingston EH, Smith VA, et al. Survival among high-risk patients after bariatric surgery. JAMA. 2011;305(23):2419-2426. http://jama.ama-assn.org/content/305/23/2419.full
7. Padwal R, Klarenbach S, Wiebe N, et al. Bariatric surgery: a systematic review of the clinical and economic evidence. J Gen Intern Med. 2011;26(10):1183-1194. http://www.springerlink.com/content/k48h0686338u7012/

One comment on “Is There a Long-Term Mortality Benefit From Bariatric Surgery?”
Great article,
Here is the latest Clinical research and news on trials. NICE guidelines, tools & resources for you to keep up-to-date in Medical & Primary Care.
Comments are closed.