Faculty Peer Reviewed
While your weekend may have been filled with Irish Soda bread, beer and college basketball, this week’s journals were heavy on the reproductive system and cancer screening and prevention.
With ever-changing recommendations, many doctors may find themselves confused when it comes to cancer screening in daily practice. As described in last week’s Primecuts, a recent paper in the Annals of Internal Medicine confirmed that many US doctors really do not understand cancer screening statistics. [1]
Screening for prostate cancer remains controversial. The United States Preventative Services Task Force (USPSTF) renewed this debate in October 2011 with the release of a new draft guideline recommending against regular screening with prostate-specific antigen (PSA) in healthy men. [2]
A study published this week in the New England Journal of Medicine is sure to add fire to the debate. According to the European Randomized Study for Screening for Prostate Cancer, patients screened with prostate-specific antigen had reduced mortality. [3] This study randomly assigned 162,388 European men between the ages of 55 to 69 to either a screening group that was offered PSA-based screening every 4 years or a control group, not offered screening. A PSA level above 3.0 ng/mL was considered positive and was followed by a recommendation for prostate biopsy. Of the men who received a screening PSA, 16.6% had a positive result and 85.9% of those with a positive result underwent prostate biopsy. After a median 11 years of follow-up, the screening group experienced a 21% reduction of prostate cancer mortality relative to the control group (RR 0.79, P=0.001). [3] According to the study, 1055 men needed to be screened and 37 prostate cancers detected to prevent one death from prostate cancer at 11 years’ follow-up. There was no significant difference in all-cause mortality. [3] Despite two years of additional data, these findings did not differ significant from the group’s previous findings from 2009 [4]. The authors do remark that there are risks associated with prostate biopsy, and there is an approximately 50% rate of cancer overdiagnosis. Their findings also conflict with the findings of a large US-based randomized controlled trial, the Prostate Lung Colorectal and Ovarian (PLCO) Cancer Screening Trial, which found no benefit from screening with PSA and digital rectal exam in men after 13 years of follow-up [5]. Thus, more information on cost-effectiveness, risks, and benefits is needed to make a general recommendation.
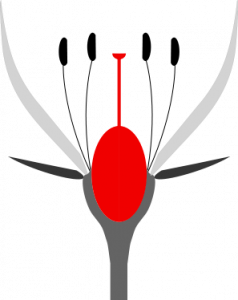
Speaking of prostate cancer, a case-controlled study published in Cancer suggests that circumcision may be protective against prostate cancer. [6] The study looked at about 1750 men with prostate cancer and 1650 men without prostate cancer from Washington State. After adjusting for confounders (age, race, family history of prostate cancer, self-reported history of sexually transmitted infections or prostatitis, study, income level and education), circumcision before first sexual intercourse was associated with a 15% reduced risk of prostate cancer compared to uncircumcised men or men with circumcision after intercourse (95% CI, 0.73-0.99). [6] Citing evidence that circumcision has been linked to decreased rates of sexually transmitted infections, the authors claim that their study supports the hypothesis of an inflammatory or infectious pathway in the development of prostate cancer. [6] This analysis, however, is observational and cannot identify any causal relationship between circumcision and prostate cancer; it will likely not affect current recommendations for or against circumcision.
Enough about men, what about women? In an early-release article published in the Annals of Internal Medicine this week, The USPSTF now recommends routine PAP smears no more frequently than every 3 years. [7] Using information from their systematic review, the USPSTF recommends the following screening:
1. Women aged 21 to 65 without known risk factors (DES exposure, immunodeficiency, prior high grade lesions) every three years with cytology only; or
2. Women older than 30 to 65 every 5 years using a combination of cytology and HPV testing.
They recommend against cervical cancer screening in:
1. All women under 21;
2. Women older than 65 who have had adequate prior negative screening; and
3. Women with prior hysterectomy and no cervix, if they have no prior history of high-grade precancerous lesions (CIN 2 or 3 or cervical cancer).
The task force also recommends against HPV testing in women under 30. They also found no difference in screening with liquid-based cytology compared with conventional cytology. In a departure from previous recommendations, no women under 21 should be screened even if they are 3 years post-coitarche.
Identification of precancerous cervical lesions in women younger than 21 and low-risk women older than 65 often qualifies as overdiagnosis; many lesions will regress and others are too indolent and slow-growing to be clinically significant. [7] The USPSTF recommendations cite increased harm and no additional benefit with excessive screening PAP smears. These harms include unnecessary anxiety, colposcopies, and biopsies with false positives. Additional risks include adverse pregnancy outcomes after cold-knife conization and loop excision, which are often used to treat precancerous lesions. [7]
These new recommendations were echoed in similar recent recommendations by the American Cancer Society, American Society for Colposcopy and Cervical Pathology and American Society for Clinical Pathology Screening Guidelines [8] and will likely lead to changes in clinical practice in screening for cervical cancer.
Cancer screening practices remain controversial. The release of more conservative recommendations over the last few years has led to a backlash as the public blames financial incentives and “death panels†for the changes. Like the public, many doctors have a poor understanding of the statistics behind cancer screening. [1] To limit the harm from false positives and overdiagnosis, medical professionals must understand the reasoning behind cancer screening recommendations and be able to explain the risks and benefits to their patients.
Pansy Tsang is a second year resident at NYU Langone Medical Center
Peer reviewed by Michael Poles, MD, Section Editor, Clinical Correlations
Image courtesy of Wikimedia Commons
References:
1. Wegwarth O, Schwartz LM, Woloshin S, Gaissmaier W, Gigerenzer G. “Do Physicians Understand Cancer Screening Statistics? A National Survey of Primary Care Physicians in the United States.†Ann Intern Med. 2012 March 6. 156: 340-349. http://annals.org/content/156/5/340.abstract
2. Chou R, Croswell JM, Dana T, Bougatsos C, Blazina I, et al. “Screening for Prostate Cancer: A Review of the Evidence for the U.S. Preventative Services Task Force.†Ann Intern Med. 2011 Oct; 155: 762-771. http://www.annals.org/content/155/11/762.abstract?sid=4f8178d2-c506-4127-be3b-aaf428644d2b
3. Schroder FH, Hugosson J, Roobol MJ, et al. Prostate-cancer mortality at 11 years of follow-up. N Engl J Med. 2012 March 15; 366:981-990. http://www.nejm.org.ezproxy.med.nyu.edu/doi/full/10.1056/NEJMoa1113135
4. Schroder FH, Hugosson J, Roobol MJ, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med 2009 Mar 26 ;360:1320-1328. http://www.nejm.org.ezproxy.med.nyu.edu/doi/full/10.1056/NEJMoa0810084
5. Andriole GL, Crawford ED, Grubb RL III, et al. Prostate cancer screening in the randomized Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial: mortality results after 13 years of follow-up. J Natl Cancer Inst 2012 Jan 18;104:1-8. http://jnci.oxfordjournals.org.ezproxy.med.nyu.edu/content/104/2/125.full
6. Wright JL, Lin DW, Stanford JL. “Circumcision and the risk of prostate cancerâ€. Cancer. 2012 March 12. Epub ahead of print. http://onlinelibrary.wiley.com.ezproxy.med.nyu.edu/doi/10.1002/cncr.26653/abstract;jsessionid=7CB2DD2 FA2FAF4A218E6396DCC49261F.d01t04
7. Moyer VA, USPSTF, “Screening for Cervical Cancer: U.S. Preventative Services Task Force Recommendation Statementâ€. Ann Intern Med. 2012 March 14. epublished early release article. http://www.annals.org/content/early/2012/03/14/0003-4819-156-12-201206190-00424?aimhp
8. Saslow D, Solomon D, Lawson HW, Killackey M, Kulasingam SL et al., “American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology Screening Guidelines for the Prevention and Early Detection of Cervical Cancer.†Ca Cancer J Clin. 2012 Mar 14; 00:000-000. Epub ahead of print. http://onlinelibrary.wiley.com/doi/10.3322/caac.21139/full

One comment on “Primecuts – This Week In The Journals”
Wright’s finding “circumcision before first sexual intercourse was associated with a 15% reduced risk of prostate cancer compared to uncircumcised men or men with circumcision after intercourse (95% CI, 0.73-0.99).” should actually read, “uncircumcised men AND men with circumcision after intercourse” since that was a pooled result. Separately they did not reach significance, and in fact such signicance as any measure reached was marginal. 15% is the relative risk ratio, which makes a small difference look large. The absolute risk ratio was 2.7% and estimates of the NNT range from 42 to 245 – scores of babies circumcised in vain to prevent one man from getting prostate cancer about 80 years from now. Yet another example of circumcision being a “cure” in search of a disease.
Comments are closed.