Faculty Peer Reviewed
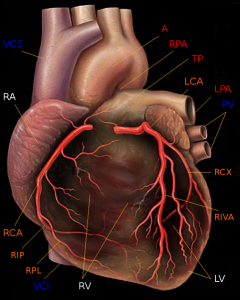
First up, the debate between coronary revascularization and optimal medical management continues. Over the past several years, the role of fractional flow reserve (FFR), a technique used during angiography to assess the functional significance of lesions seen on coronary angiography, has begun to be established. A study published in the NEJM this week looked specifically at the role of FFR in patients with stable coronary artery disease. 1220 patients with stable coronary artery disease and lesions appropriate for percutaneous coronary intervention (PCI) were enrolled, and of the 888 with at least one lesion with an FFR less than 0.80, 447 were randomized to PCI with drug-eluting stent plus medical therapy and 441 medical therapy alone. Medical therapy included aspirin, a beta-blocker, an ACEI or ARB, and a statin; patients who underwent PCI were also treated with clopidogrel. The primary end point was a composite of death, MI, or urgent revascularization; secondary end points included non-urgent revascularization and angina class.
Mean follow-up time was a little over seven months; the study was terminated early due to an increased event rate in the medical therapy arm. The difference in the incidence of the primary outcome, 12.7% in the medical therapy arm versus 4.3% in the PCI arm (hazard ratio 0.32), was driven mainly by the need for urgent revascularization in the medical therapy arm. Individually, there were no differences in the rate of death or MI between the two groups. Subgroup analysis showed that PCI patients with an FFR below 0.65 seemed to have an even more pronounced benefit from intervention. By landmark analysis, the beneficial effects of PCI were seen more frequently a week after randomization, leading the authors to speculate that even greater effect may have been observed with more follow-up time. Limitations included the ability to account for in-stent restenosis given the relatively short follow-up time, the absence of aggressive interventions for risk factor reduction in the medical therapy arm that had been employed in previous studies, and the absence of clopidogrel treatment in the medical therapy arm. The authors suggest that taken together, the data imply that treating functionally significant coronary artery lesions with stent revascularization is a better management strategy than medical therapy alone.
Now we shift gears to another common disease, asthma, and the role of chronic corticosteroid therapy in disease management. Traditionally, doses of corticosteroid inhalers are adjusted by physician judgment; this study was designed to test the hypothesis that using patient symptoms alone (as determined by use of emergency albuterol inhaler) or an objective measure like exhaled nitric oxide to guide corticosteroid dosing would be a superior management strategy compared to relying on physician intervention. Previous data showed equivalent outcomes with symptom-based therapy as compared to physician-guided therapy in mild asthma. In this trial, 342 patients with mild to moderate persistent asthma that was well or partially-controlled were randomized to one of the three arms mentioned above. The primary outcome was time to first treatment failure; other markers of asthma activity including spirometry measures, sputum eosinophils, and quality of life measurements were recorded as secondary outcomes. While there was no significant difference in primary outcome at nine months among the three groups (22% for physician-based assessment group, 20% for nitric oxide based measurement group, and 15% for symptom-based therapy group), the total dose of corticosteroids administered was lower in the symptom-based group than in the other two groups. Importantly, this study noted some response differences by ethnic groups, namely that being of black or Hispanic descent correlated with shorter time to first treatment failure as compared to non-Hispanic whites.
Finally, we go back to the bench to an article in Nature published by our own Dr. Ilseung Cho and Dr. Martin Blaser. Building on the common practice of antibiotic administration to animals to promote weight gain, the authors studied the effects of subtherapeutic antibiotic treatment (STAT) in mice. They first showed mice treated with early STAT had higher total fat mass than control mice, in spite of no overall growth difference, and that these differences were noted as soon as several weeks after treatment started. STAT mice also reached higher bone mineral densities first (though this difference did not persist) and had a trend towards hyperglycemia as compared to untreated mice. The authors then looked specifically at gut microbiomes, and found that, while STAT mice did not have altered censuses of bacteria as compared to control mice, they did have a different distribution of said bacteria. The study observed that antibiotic treatment altered short chain fatty acid (SCFA) metabolism, and as SCFAs can stimulate adipogenesis, this may explain the link between antibiotic treatment and weight gain. STAT finally induced upregulation in synthesis of lipids and triglycerides. All of these effects seem proximal, as there were no differences in the actual adipose tissue of STAT versus control mice. Putting it all together, the authors hypothesize that antibiotic treatment selects for a microbiome with increased bacterial activity that extracts more calories from food (as compared to untreated mice), leading to increased short chain fatty acid metabolism and overall increased lipogenesis. Although there are many steps between studying experimental mice and treating patients in the clinic, this study nonetheless raises some very interesting questions about the effects of early antibiotic treatment, a practice observed daily on the floors of the hospital.
Other interesting papers this week:
A phase 2 study in the Lancet looking at using neonatal keratinocytes and fibroblasts found that a topical spray with these cells can heal venous leg ulcers. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(12)60644-8/fulltext
Addition of single-photon emission computed tomography/computer tomography to sentinel lymph node excision results in more extensive disease and lower relapse rates with prolonged survival in a retrospective cohort as compared to sentinel lymph node excision alone. http://jama.jamanetwork.com/article.aspx?articleid=1357261
Mutations in the phosphatase and tensin homologue (PTEN) gene, a known tumor-suppressor gene, are associated with lower insulin resistance/increased insulin sensitivity but also increased obesity. http://www.nejm.org/doi/full/10.1056/NEJMoa1113966
Dr. Lakshmi Tummala is an Associate Editor, Clinical Correlations
Peer reviewed by Neil Shapiro, Editor-In-Chief, Clinical Correlations
Image courtesy of Wikimedia Commons
References:
1. http://www.nejm.org/doi/full/10.1056/NEJMoa1205361
2. http://jama.jamanetwork.com/article.aspx?articleid=1357259
3. http://www.nature.com/nature/journal/v444/n7122/abs/nature054